Abstract
Introduction: Acute vaso-occlusive crisis (VOC) is the hallmark clinical complication of sickle cell disease (SCD). VOC involves several mechanisms, including rigid erythrocytes, adhesive blood cells, activated coagulation, activated and dysregulated endothelium, inflammation, and ischemia-reperfusion injury. Surprisingly few data document clinical and laboratory markers that change from steady state to VOC and during the hospital stay, and that predict subsequent rehospitalization. We characterized such markers in this study.
Methods: Data were collected as part of a clinical trial of nitric oxide as potential treatment for VOC (DeNOVO). Participants, age ≥ 10 years requiring hospitalization for VOC, were recruited from 11 academic medical centers at the time of VOC. Length of hospital stay (LOS), change in visual analogue scale (VAS) pain score, and hospital readmission within 30 days were study outcomes. Steady state laboratory values were available in a subgroup of patients for comparison. Differences between admission and steady state laboratory measures and changes in clinical and laboratory parameters from hospital admission to discharge were analyzed by Wilcoxon signed-rank test. Multivariate linear and logistic regression analyses were used to identify the independent predictors of LOS and 30-day readmission risk.
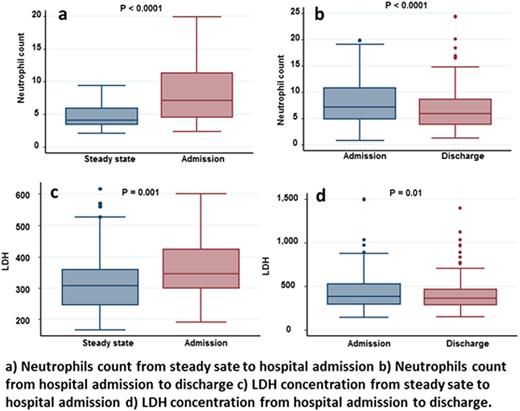
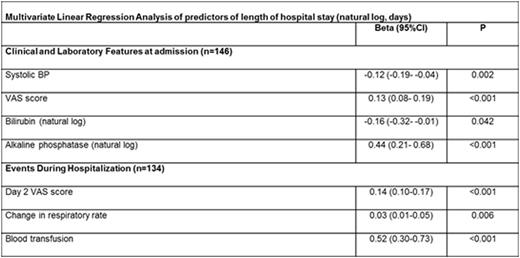
Results: 150 recruited patients had a median (interquartile range; IQR) age of 24 (17-33) years; 50% were female, and 91% had HbSS genotype. The median VAS score at time of admission was 7.7 cm which subsided to 3.3 cm at time of discharge (P <0.001). Serum lactate dehydrogenase concentrations (LDH) and neutrophils counts increased from steady state to the time of the VOC (P ≤ 0.001) and then decreased during the hospital stay (P ≤ 0.01) (Figure). The median (IQR) LOS was 3.5 (1.9-6.0) days. Longer LOS was predicted by higher admission VAS and serum alkaline phosphatase level, as well as higher increase in respiratory rate during hospital stay (P ≤ 0.006) (Table). The rate of 30-day hospital/ED readmission was 24%. Longer LOS was associated with lower risk of readmission (OR = 0.65, 95% CI: 0.50-0.86 per day). Other risk factors for readmission were higher serum creatinine at discharge (OR = 5.54, 95% CI: 1.12-27.51 per mg/dL), greater increase in serum alanine aminotransferase (OR = 1.03, 95%CI: 1.01-1.06 per unit increase) and greater cumulative opioid doses (OR = 1.25, 95%CI: 1.11-1.49 per 100 mg) during the index hospitalization.
Conclusion: VOC is associated with neutrophilia and increased LDH, consistent with inflammation and hemolysis and/or tissue injury, although of insufficient magnitude to be used as diagnostic criteria. The magnitude of pain and marker of apparent bone involvement predict longer LOS. SCD patients with VOC carry a high burden of readmission risk, which is characterized by higher opioid utilization and earlier discharge from the index hospitalization. These concepts can shape models, especially to reduce readmission rate, to be evaluated in prospective clinical trials.
*First two authors contributed equally to this work.
Lanzkron:NKT: Research Funding; Selexys: Research Funding; Prolong: Research Funding; PCORI: Research Funding; NHLBI: Research Funding; HRSA: Research Funding; GBT: Consultancy; Pfizer: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.