Abstract

Introduction: Vaso-occlusive episodes are the most common complication experienced by individuals with sickle cell disease (SCD). Treatment in an emergency department (ED) is often required and significant variability in care exists. In 2014, NHLBI published evidence based recommendations suggesting treatment with either an individualized opioid dosing or standard weight-based protocol; however the supporting evidence grade was Consensus - Panel Expertise. As outlined in the results section, the aim of this project was to compare change in pain scores, patient safety and system utilization variables between patients randomized to an individualized or weight based (standard) dosing protocol for treatment of VOC from arrival to discharge in an ED setting.
Methods: A randomized controlled trial was conducted in two EDs (OH and NY). Adults with SCD were eligible for inclusion and recruited during a hospitalization, clinic visit or at the end of an ED visit. Patients were randomized to treatment with an individualized opioid dosing protocol (developed by the SCD physician based on patients' prior opioid use) or standard weight based protocol. Both protocols were supported by the NHLBI recommendations for treatment of VOE (2014) to include repeat dosing. Protocols were made available on the electronic medical record for future ED visits (up to five visits/patient), should they occur. ED physicians were informed of the protocol and ordered analgesics. Research staff was notified when ED visits occurred for enrolled patients and obtained assessments of pain (0-100 cm VAS) every 30 minutes from placement in the ED to one of 3 study endpoints: 1) 6 hours; 2) decision to admit to the hospital; 3) discharge home. The unit of analysis was the ED visit rather than patient. The primary outcome was change in pain score from arrival to study endpoint. Research staff reviewed the medical record 30 days after the ED visit to determine secondary outcomes of hospital admission, re-admission and new ED visits within 72 hours, 7 and 30 days post the index ED visit. The medical record was reviewed for administration of narcan, intubation, or assisted ventilation. A hierarchical linear mixed effects model adjusting for nested patient and site effects were used to test for a difference in the mean pain change scores in the treatment arms. Generalized Linear Models adjusting for nested patient and site effects were performed to evaluate differences in the dichotomized secondary outcomes.
Results: 106 patients enrolled in the study with 52 patients (sites: 25 OH, 27 NY) contributing a total of 126 ED visits over 12 months. Among the 52 patients with visits, the median number of ED visits/patient was 2.0, 58% were male, and the median age was 27 years (range: 21 to 60). No patients in either treatment arm required narcan, intubation, or assisted ventilation.
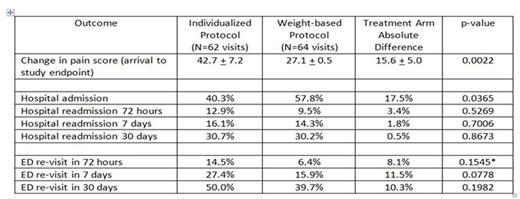
Pain change: Mixed effect model adjusted mean ± standard deviation, higher positive score = greater pain reduction; *Fisher's Exact Test result due to low cell frequency.
Conclusions: An individualized opioid dosing protocol resulted in a larger reduction in pain scores and lower hospital admission rate among patients with SCD treated for VOE in two EDs when compared to treatment with a weight-based opioid protocol. However, there was a tendency for more frequent ED re-visits within 72 hours, 7 and 30 days among patients in the individualized opioid dosing protocol. A pragmatic RCT with a larger and more heterogeneous sample of patients and ED settings is required to provide definitive evidence to guide treatment of VOE.
Tanabe:NHLBI: Research Funding. Bosworth:WestMeadVaco: Research Funding; CVS carematix: Consultancy; Improved Patient Outcomes: Research Funding; Johnson & Johnson: Consultancy, Research Funding; Genentech: Consultancy; sanofi: Honoraria, Research Funding; Pharma Foundation: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract