Abstract
Background: Behçet disease (BD) is a systemic chronic vasculitis, in which Th 1 polarized immune response and plays a major role in the pathogenic process. The anti-TNFα, is the highest effectiveness treatment, but presents some limitations such as high costs and side effects. Recently, platelets have shown emerging role as immune cells with multiple inflammatory and immune regulators proteins. The aim of this study was to characterize autologous PRP of patients with BD, and evaluate its effects as immunomodulator through its subcutaneous application.
Methods: Eight patients with BD were evaluated in over a year. PRP therapy was applied during six months with a total of 9 PRP injections (first 6 every two weeks, last 3 monthly). Immunomodulation provide by platelets was assessed in five time points: basal, 3 (3M), 6 (6M), 9 (9M) and 12 (12M) months after the first PRP injection. Patients samples were evaluated to: frequency of effectors T cells (CD4+; CD8+), regulatory T cells (CD4+, CD25+,FOXP3+), activated/no activated NK cells (CD 69+CD56+), (CD16+CD56+), cytokines profile such as TNF-α, IFN-γ IL-1β, IL-2, IL-6, IL-8, IL-10, IL-12, IL-13, IL-17, IL-21, PF4, CD40L by CBA, and growth factors (GF) TGF-β, PDGF, EGF, and VEGF through Luminex. PRP was characterized regarding number of leukocytes, platelets and the same cytokines and growth factors analyzed in plasma samples.
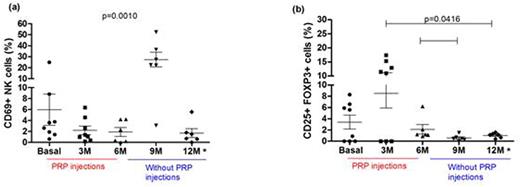
Results: PRP were concentrated in a median of 5 folds related to the basal of platelet numbers, demonstrating a high recovery of platelets. The median of leukocytes cells were 0.5 folds related to their basal number that evidenced a poor concentration of leukocytes in the PRP. PRP GF maintained similar levels during the treatment, except for a significantly increase of TGF-β1 (p<0.0001) and decrease of IL-10 (p=0.0088). We observed a significant increase of regulatory T cells (p=0.0416), especially for the first 3 months: median of basal time 3.25% (from 0 - until 8.3%); median of 3M: 11.25% (from 0 - until 17.4%). A significant decrease of inflammatory profile was observed, especially for activated NK cells, a marker of disease activity (p=0.0010): median of basal 3.1% (from 0.6 - until 24.9%), median of 3M: 1.25% (from 0.2 - until 6.4%), figure 1. After 3 months of last PRP injection (9M) a shift of patients pattern response was observed, with a significantly increase of inflammatory cells, specially increase of activated NK cells [median of 9M: 25.0% (from 3.1% - until 52.4%)] and decrease of regulatory T cells [median of 9M: 0.48% ( from 0.02% - until 1.5%)]. Clinically at 9M the patients presented worsening of the disease and received high doses of corticoids. Interestingly, IL-10 which has a pattern of high concentration in plasma samples of BD patients when compared with health individuals, presented a significant decrease after 6 months, (p<0.0001) with a median of basal time 241.8 fg/ml and a median of 9.1 fg/ml for 12M. The IL-8, which could shows an increase of levels during the disease progression, reached a significantly minor value at 9 months (p=0.0459), with 344.8 fg/ml (52.4 - 2596 fg/ml), when compared with basal time of 1797.0 fg/ml (508.6 - 4385 fg/ml).
Conclusion: As a very interesting and novel finding we evidenced that autologous subcutaneous injections of PRP showed an immunomodulation in BD patients. The inflammatory profile decreases, whereas the regulatory profile increased during PRP injections. The autologous PRPs were extensively characterized, especially for GF and PF4. The first one presents a role in angiogenesis, adhesion molecule expression and PF4 is a chemokine that in turn interacted with monocytes, neutrophils, T-cell recruitment and Th differentiation. We could observe that the frequency of PRP injections and period of action is determinant for biologic effect. The best results were obtained along 3 months of treatment with an interval of 15 days between PRP injections. The advantage of PRP when compared to biological therapy available, such as anti-TNF-α, is the low cost, no immunogenicity and minor side effects. This study suggested a beneficial effect of autologous PRP therapy on biologic profile of BD patients and encourages the development of trials with higher number of patients in randomized studies to analyze clinical efficacy and safety.
The frequency of activated NK cells (a) and regulatory T cells (b) in plasma samples of patients. * Patients were in use of higher doses of corticoids.
The frequency of activated NK cells (a) and regulatory T cells (b) in plasma samples of patients. * Patients were in use of higher doses of corticoids.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.