Abstract

Introduction: Paroxysmal nocturnal hemoglobinuria (PNH) is an acquired stem cell disorder with the expansion of PIGA mutant clone(s), which is deficient in GPI-anchored proteins including CD55 and CD59. The lack of CD55 and CD59 renders PNH-type red blood cells (RBC) susceptible to complement attacks, resulting in intravascular hemolysis. Classic PNH manifests 3 major symptoms: anemia, bone marrow failure, and thrombosis. Small populations of PNH-type cells (<1.0%) have been found in approximately 60% of aplastic anemia (AA) and in 20% of low-risk myelodysplastic syndrome (MDS) patients with no clinical or biochemical evidence of hemolysis. The presence of increased PNH-type cells in bone marrow failure (BMF) patients was shown to predict better response to immunosuppressive therapy by retrospective (Blood 2006 107:1308-1314) and prospective (Br J Haematol 2014 164:546-54.) studies. To ascertain the clinical significance of PNH-type cells, we conducted a nationwide, multicenter, prospective, observational clinical study named OPTIMA in Japan.
Methods: Patients diagnosed with PNH, AA, MDS or indistinguishable BMF were prospectively recruited to the study since 2011 in Japan. A high-resolution FCM assay was established to precisely detect a small population of PNH-type granulocytes (with FLAER) and RBCs (with anti-CD55 and CD59 antibodies) ≤ 0.01% of the total granulocyte or RBC population based on the Kanazawa method (Blood 2006 107:1308-1314). Six university laboratories across Japan were designated as regional analyzing centers and measured the percentages of PNH-type cells in the study population, as well as collected clinical and laboratory data. Periodic blind cross validation tests using a positive control sample containing 0.01% PNH-type cells and a negative control sample were performed to minimize inter-laboratory variations.
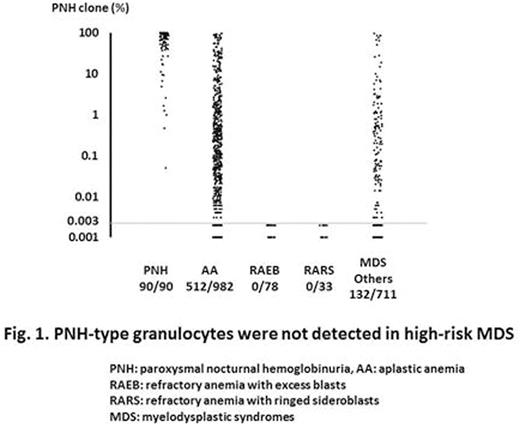
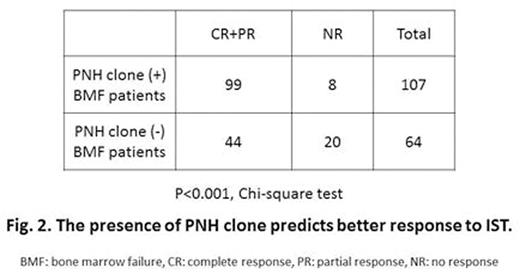
Results: As of July 2016, 2,849 patients were enrolled in the study and 2,734 patients were analyzed. Nine hundred twelve patients (33.4%) were positive for PNH-type cells (≥ 0.005% PNH-type erythrocytes and/or ≥ 0.003% PNH-type granulocytes) and 238 (8.7%) patients had more than 1% of PNH-type cells. PNH-type cells were positive in 90/90 PNH (100%), 512/982 AA (52.1%), 132/822 MDS (16.1%), and 141/512 indistinguishable BMF (27.5%) patients. Among the MDS patients, PNH-type cells were positive in approximately 20% of patients with RCUD, RCMD, MDS-U, or 5q- syndrome, but not in any patients with RARS, RAEB-1, and RAEB-2 (Fig. 1). The serum LDH level increased in proportion to the PNH clone size of RBCs, and 63.3% of the patients possessing ≥1.0% RBCs showed LDH levels more than 1.5 times the upper limit of normal. Of 171 patients who completed submission of 3-year follow-up data, BMF patients with PNH-type cells showed a better response rate [CR+PR, 99/107 (92.5%)] to IST compared to those without PNH-type cells [44/64 (68.8%)] (P<0.001, Chi-square test) (Fig. 2).
Conclusions: These interim analyses of the OPTIMA study demonstrate that our high-resolution FCM is reliable in detecting small populations of PNH-type cells and produces consistent results among different laboratories. The presence of PNH-type cells exclusively in patients with AA and low-risk MDS suggests a link between benign pathophysiology of BMF and an increase in the number of PNH-type cells. The better response of PNH-type cell-positive BMF to IST compared to BMF without PNH-type cells was consistent with previous reports. Our data, for the first time, prospectively confirms the significance of small populations of PNH cells in BMF patients in Japan and warrants further worldwide, prospective studies on non-Japanese patients with BMF.
Ueda:Alexion Pharmaceuticals: Honoraria, Research Funding. Nishimura:Alexion Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Hosokawa:Aplastic Anemia and MDS International Foundation: Research Funding. Yonemura:Alexion Pharmaceuticals: Research Funding. Obara:Alexion Pharmaceuticals: Honoraria, Research Funding. Shichishima:Alexion Pharmaceuticals, Inc. Japan: Honoraria. Ninomiya:Alexion Pharmaceuticals: Honoraria. Kawaguchi:Alexion Pharmaceuticals: Honoraria. Kanakura:Fujimotoseiyaku: Research Funding; Toyama Chemical: Research Funding; Bristol - Myers: Research Funding; Nippon Shinyaku: Research Funding; Astellas: Research Funding; Eisai: Research Funding; Pfizer: Research Funding; Chugai Pharmaceutical: Research Funding; Shionogi: Research Funding; Kyowa Hakko Kirin: Research Funding; Alexion Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau. Nakao:Alexion Pharmaceuticals: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract