Abstract
Background
Patients with solid tumors treated at a National Cancer Institute designated cancer center (NCI-CC) have been found to have improved survival when compared to those treated elsewhere. Few population-based studies have evaluated the association between location of care, complications associated with intensive therapy and early mortality (defined here as death ² 60 days from diagnosis) in patients with AML.
Methods
Using linked data from the California Cancer Registry and Patient Discharge Dataset from 1999 to 2012, we identified patients ³15 years of age diagnosed with AML who received inpatient treatment. Hospitals where patients received their care were classified as either NCI-CC or non-NCI designated facilities (non-NCI-CC). Logistic regression was used to estimate associations between patient characteristics (age, sex, race/ethnicity, year of diagnosis, marital status, neighborhood socioeconomic status, health insurance, and medical comorbidities) and location of care (NCI-CC vs non-NCI-CC facilities), and then to build a propensity score. Inverse probability weighted logistic regression models were used to determine associations between location of care and complications with early mortality. Interactions of complications and location of care with early mortality were also considered. Results are presented as adjusted odds ratios (OR) and 95% confidence intervals (CI).
Results
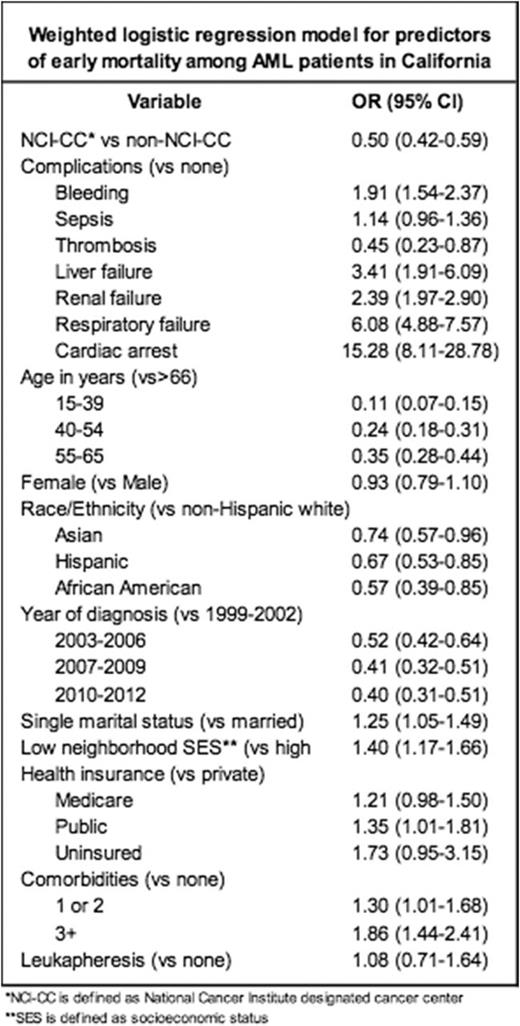
Of the 5613 patients with AML identified, 1406 (25%) were treated at an NCI-CC. Compared to patients treated elsewhere, AML patients treated at an NCI-CC were more likely to be <65 years of age, Hispanic (versus non-Hispanic white), live in higher socioeconomic status neighborhoods, have fewer comorbidities and have Medicare or public (versus private) health insurance. Patients treated at NCI-CCs had higher rates of renal failure (21% vs 18%, P=0.03) and lower rates of respiratory failure (11% vs 14%, P=0.002) and sepsis (33% vs 36%, P=0.04) than those treated at non-NCI-CCs. Rates of bleeding, thrombosis, liver failure and cardiac arrest did not differ by location of care. After propensity-score weighting, baseline characteristics were balanced between patients treated at NCI-CCs versus non-NCI-CCs (all standardized mean differences <2.3%). In multivariable, inverse probability weighted models, treatment at an NCI-CC (versus non-NCI-CC) was associated with lower early mortality (OR 0.50, CI 0.42-0.59) (Table). Complications associated with higher early mortality, regardless of treatment location, included: bleeding (OR 1.91, CI 1.54-2.37), liver (OR 3.41, CI 1.91-6.09), renal (OR 2.39, CI 1.97-2.90) and respiratory (OR 6.08, CI 4.88-7.57) failure and cardiac arrest (OR 15.28, CI 8.11-27.78) (Table). The impact of complications on early mortality did not differ by location of care with the exception of respiratory failure (P for interaction=0.001); AML patients with respiratory failure had a higher odds of early mortality when treated at non-NCI-CCs (OR 8.59, CI 6.66-11.07) versus NCI-CCs (OR 4.43, CI 2.68-7.33). Other factors significantly associated with early mortality included younger age, treatment after 2002, non-Hispanic White race/ethnicity (versus African Americans, Hispanics and Asians), single marital status (versus married), residence in low socioeconomic status neighborhoods (versus high) and presence of any comorbidities (versus none).
Conclusions
In patients with AML, initial treatment at a NCI-CC is associated with 50% reduction in early mortality than treatment at a non-NCI-CC, adjusted for baseline socio-demographic variables, comorbidities and complications within 60 days. Lower early mortality may result from differences in supportive care practices, hospital or provider experience and access to clinical trials at NCI-CCs. Future studies should evaluate the specific differences in care at NCI-CCs to inform strategies to improve early mortality outcomes for all AML patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.