Abstract

Platelet transfusion refractoriness (PTR) is defined by the repeated failure to appropriately increment platelet count after platelet transfusion. PTR represents a real concern in the management of patients (pts) who require iterative platelet transfusions, in particular those undergoing intensive treatment (Stanworth, Br J Haematol 2015). PTR can be secondary to non-immune and immune causes and is associated with adverse events including longer hospital stays, severe hemorrhages and increased risk of early deaths. After induction chemotherapy for acute myeloid leukemia (AML), intensive transfusion support is required during the 4-6 weeks of treatment-induced aplasia. There is few data regarding management and outcome of AML pts with PTR in this setting.
This study included all consecutive pts treated by intensive chemotherapy for non-promyelocytic AML in Toulouse University Hospital between January 2001 and December 2014 who developed PTR during the induction phase. Platelet count is measured daily and transfusion of ABO-identical platelets is performed when <10.109/L according to standard guidelines. We pragmatically used a clinical definition of PTR, ie. persistent thrombocytopenia <10.109/L despite at least two successive daily platelet transfusions. Control patients were those treated by intensive chemotherapy without PTR. Intensive chemotherapy consisted in daunorubicin (60-90 mg/m² d1-3) or idarubicin (8 mg/m² d1-5) with cytarabine (100-200 mg/m² d1-7); lomustin being added in pts > 60y.
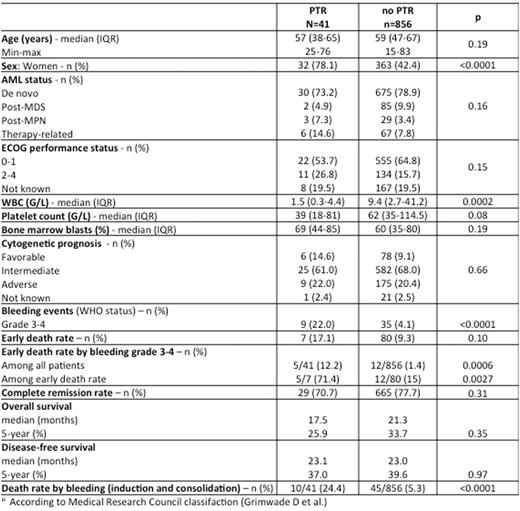
We identified 41 cases of PTR among 897 pts in our database (4.8%; 2.9 patients/y). PTR patients were mostly women (78.1% vs 42.4% in non-PTR pts, p<0.0001), with a median age at diagnosis of 57y vs. 59y in non-PTR (table). PTR pts had more often splenomegaly which is a classical factor associated with PTR (22% vs 8.5%, p<0.009). PTR-AML were de novo in 73.2% of cases (only 10 pts had received platelet transfusions prior to initiation of the induction therapy [24.4%]), with cytogenetics and molecular abnormalities not significantly different to non-PTR AML (favorable/intermediate/adverse karyotype: 14.6/61/22% vs 9.1/68/20.4%,; NPM1 mutations: 33.3% vs 33%; FLT3-ITD mutations: 9.7% vs 22.8%). Anti-HLA antibodies were identified in 34/40 PTR pts (82.9%). The median time from chemotherapy initiation to PTR diagnosis was 10.5 days (IQR, 6-16.5). The median duration of thrombocytopenia (from PTR diagnosis to the first platelets count > 50.109/L) was 19 days (IQR 15 - 25.5).
Management of PTR-pts was as follows: a twice-daily prophylactic transfusion strategy in 30 pts (73.2%) regardless of bleeding events, one or more HLA-matched platelet transfusion in 15 pts (83.3% of 18 patients with matched donors), corticosteroids (n=15, 36.6%), intravenous immunoglobulins (n=14, 34.2%), TPO agonists (n=10, 24.4%) or rituximab (n=1). Median time between PTR diagnosis and first HLA-matched platelet transfusion was 12.5 days (IQR, 6.5-15).
There were 7 early deaths in the PTR group (17.1%) compared to 80 (9.3%) in the non-PTR group (p=0.1). Grade 3-4 bleeding events during induction, early death rate (before end of aplasia) by grade 3-4 bleeding and death rate by bleeding regardless of the phase of treatment (induction+consolidation) were significantly higher in the PTR group (respectively 22% vs 4.1%, p<0.0001, 12.2% vs 1.4%, p<0.0006 and 24.4% vs 5.3%, p<0.0001). However, there was no significant difference in 5-year overall survival between both groups (25.9% vs 33.7%, p= 0.35).
HLA-matched transfusions have induced an increment in platelet count >10.109/L in 37% of cases.TPO agonists did neither shorten PTR duration (11.5 days with TPO agonists [IQR, 5.5-15] vs. 10.5 days [IQR, 6-16.5]), nor reduce severe bleeding or early death rate (40% and 20% with TPO agonists vs. 21.9% and 17.1% without).
PTR during induction therapy for AML pts significantly increases the risk of early and late deaths by severe bleeding. While TPO agonists did not appear as a relevant strategy for PTR pts, the efficacy of both massive prophylactic and HLA-matched transfusion could have reduced the risk of severe bleeding but remains to be clearly established. Since steroids, immunoglobulins or even rituximab did not prove efficacy in this setting, a better understanding of platelet destruction is needed to design mechanism-based therapeutic strategies for this very high risk condition.
Tavitian:Novartis: Membership on an entity's Board of Directors or advisory committees. Huguet:Pfizer, Novartis, BMS, Ariad, Jazz, Amgen: Membership on an entity's Board of Directors or advisory committees. Récher:Celgene, Sunesis, Amgen, Novartis, Chugai: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract