Abstract
Introduction: Postremission treatment in adult acute myeloid leukemia (AML) is mandatory to improve long-term remission duration. Allogeneic stem-cell transplantation (allo-SCT) is considered gold standard in younger patients (pts) with higher risk of relapse, whereas in pts categorized as standard-risk (SR) AML the optimal treatment remains an open issue. High-dose cytarabine (HD-ARAC) is considered the backbone of postremission treatment in SR AML. The optimal dose and schedule, and the clinical benefit of additional chemotherapeutic agents remain controversial (Schaich, 2011- Lowenberg, 2011- Lowenberg, 2013) as well as the relative efficacy of HD-ARAC in the different cytogenetic and molecular subgroups of SR AML. We analyzed the very long term outcome of consecutive unselected AML pts treated according to AML 00 NILG protocol (Bassan, Blood, 2003: 102; 11) with three repetitive HD-ARAC-based cycles, associated with idarubicin, followed by limited peripheral blood stem cell (PBSC) support, in order to reduce toxicities.
Methods: We evaluated 263 consecutive AML pts, diagnosed at our Institution, from January 2001 to March 2016 (median age 52 years - range 15-65). The treatment plan included induction with ICE (Idarubicin-Cytarabine-Etoposide) followed by IC consolidation or HD-ARAC/HD-idarubicin (SPLIT therapy) in refractory cases. ARAC 1g/mq bd for 4 days (A8) was given to CR pts, to collect 3-6x10^6 CD34/kg in 3 aliquots. Patients with ELN favorable or intermediate risk AML, considered SR AML, received 3 cycles of HD-ARAC (2g/mq bd for 5 days) plus idarubicin (8mg/mq for 2 days) with PBSC reinfusion (1-2x10^6 CD34/Kg) (A20). The pts with insufficient CD34 cells yield, received 2 courses HD-ARAC (1g/mq bd for 5 days) plus idarubicin (10mg/mq day 1) (A10). The cumulative dose of ARAC and idarubicin given according to A20 protocol were 69,4 g/mq and 162 mg/mq, respectively.
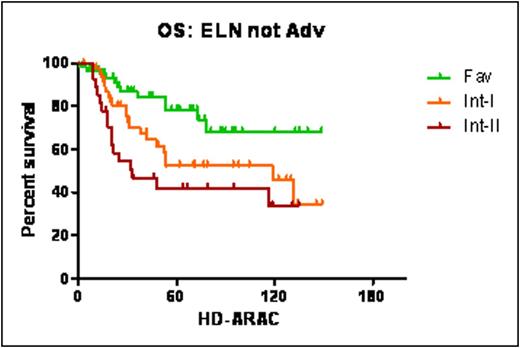
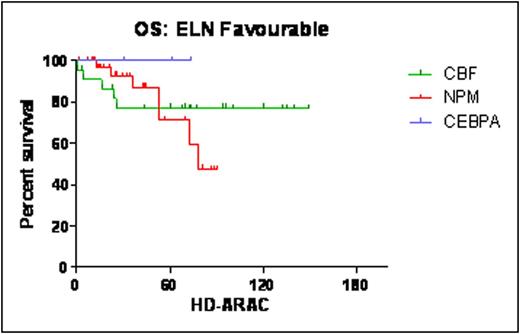
Results: Among 263 pts, 142 (54%) pts were considered SR and 116 (44.1%) HR. Only 5 pts were lacking molecular or cytogenetic information (1.9%) to allow ELN risk classification. Accordingly, 65 pts (25.2%) were favorable [35.4% core binding factor (CBF) positive, 9.2% CEPBA mutated and 55.4% NPM mutated], 87 (33.7%) Intermediate-I, 45 (17.4%) Intermediate II and 61 (23.7%) adverse risk. CR rate after ICE treatment was 77.6% (204/263), 95.8% in SR and 56% in HR pts and after ICE+SPLIT it was 88.2% (232/263); early or aplastic death was 6%. A8 course was administered in 218 pts, of whom 179 were successfully mobilized (82.1%). Among 136 SR pts, 127 were received HD-ARAC (A20 or A10), 4 allo-SCT for early relapse, 3 pts did not proceed to A20 because of prolonged cytopenia and 2 are ongoing. Hematological toxicity was acceptable. ANC recovered at a median of 10 days after CD34+ cells reinfusion. Two death in CR occurred within 100 days after A20 therapy (1.6%). After a median follow-up of 53.3 months (range 1-172), the median survival of SR AML patients was 118.9 months, the DFS and OS at 5 y were 51+/-4.8% and 56.5+/-4.7%, and at 10 y 43.3+/-5.9% and 49.6+/-5.7%, respectively. According to ELN risk, the OS at 5 y and 10 y was 78.3+/-6% and 68+/-8.7% in favorable (median OS not reached), 52.3+/-8% and 46+/-9.4% in Intermediate-I (median OS 118.8 months), and 42+10% and 33.6+/-10.9% in Intermediate-II (median OS 33.1 months) (p0.0034) (Figure1). According to molecular characteristics, the OS at 5-y was 100% in CEBPA-mutated, 77+/-9% (+/-SE) in CBF-mutated and 71+/-11% in NPM-mutated subgroups, respectively (Figure 2). In NPM-mutated pts it was 56+/-14% if FLT3 was mutated and 75+/-10% if not. At 8-y OS was not evaluable in CEBPA-mutated, it remained 77+/-9% in CBF mutated but dropped to 47+/-15% in NPM-mutated pts due to late relapses (28%), which occurred in pts without FLT3. The median time to relapse in NPM pts was 17 m, the latest relapse occurred after 97 months.
Conclusion: A postremission program with repeated courses of HD-ARAC associated to idarubicin and limited autologous CD34+ cells support was feasible, well tolerated and very effective, also long-term, in pts with ELN favourable or intermediate risk AML. The late relapse tendency of NPM-mutated AML is puzzling and should be considered by innovative programs aimed at improving these results.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.