Abstract
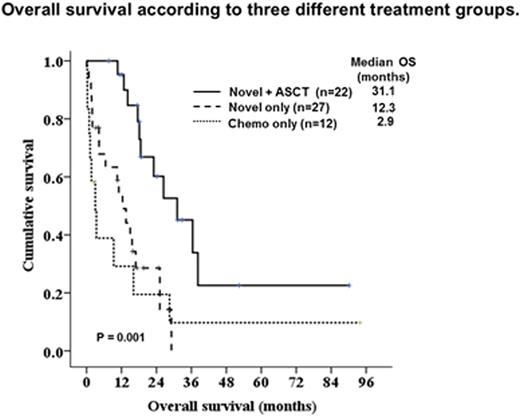
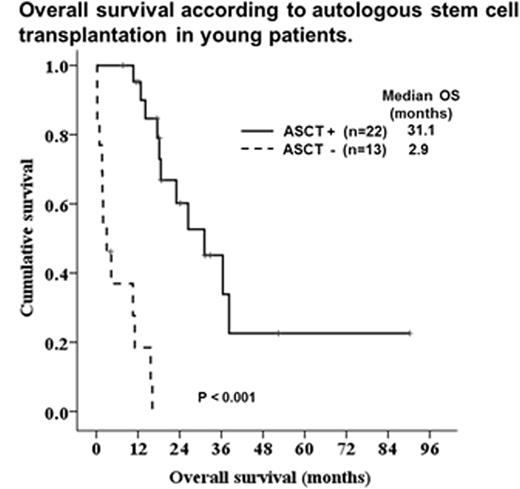
Primary plasma cell leukemia (pPCL) is a rare and aggressive plasma cell neoplasm, with rapid clinical course. In this study, we evaluated the treatment status and survival outcomes of Korean patients with pPCL. Seventy patients were diagnosed with pPCL between February 1998 and December 2015. The median age of the patients was 63.5 years (range, 34-85). Most of patients (70.0%) had International Staging System III.Conventional karyotyping was assessed in 47 patients and FISH analysis was performed in 43 patients. Abnormal karyotype was detected in 34 patients (72.3%). The most common abnormalities were complex karyotype (65.9%). Hypodiploidy, del (13q14), del (17p13), and t(11;14) were found16 (34%), 14 (29%), 12 (25%), and 11 (23%) patients, respectively. Amongthe 70 patients, 60 patients were treated.Thirty-six patients were initially treated with novel agents and 12 received novel-containing regimens as salvage therapy. Twelve patients received conventional chemotherapies only. Twenty-two patients underwent high dose chemotherapy and autologous stem cell transplantation (HDT/ASCT), and one received the allogeneic stem cell transplantation. After a median follow-up of 16.5 months, overall survival (OS) was 16.1 months (95% CI, 11.7-20.8). Twenty patients (33.3%) died within less than one year following the diagnosis, and the early mortality rate was lower in patients who were initially treated with novel agents (22.2% vs. 50.0%, p = 0.049). The median OS of three treatment groups comprising conventional chemotherapy only, novel agents only, and novel agents + HDT/ASCT were 2.9, 12.3, and 31.1 months, respectively (P=0.001). Patients who achieved complete response (CR)after initial therapy had significantly improved OS than did others (36.4 vs. 14.1 months, P < 0.011). On multivariate analysis, achievement of complete response (CR) after induction therapy (HR 0.066, 95% CI 0.007-0.615, P = 0.017), increased lactate dehydrogenase (HR 4.803, 95% CI 1.202-19.186, P = 0.026), andserum beta2-microglobulin > 5.5 mg/dl (HR 3.218, 95% CI 1.011-10.238, P = 0.048)were significantly associated with survival outcomes. In young patients (age < 65 years), performance of HDT/ASCT (HR 0.038, 95% CI 0.004-0.381, P = 0.005) was significantly associated with improved OS. In conclusion, patients with pPCL had poor survival outcomes, and achieving CR after induction therapy associated with increased OS. In addition, performance of HDT/ASCT is important treatment modality to improve OS in young patients with pPCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.