Abstract
Background: Matching for all alleles of the HLA-A, -B, -C, and -DRB1 loci (8/8 match) is associated with the highest overall survival (OS) rates after unrelated donor (URD) hematopoietic stem cell transplantation (HSCT). In Europe, patients (pts) are also matched at the HLA-DQB1 loci (10/10 match) with no overall evidence of improved OS. HLA-DPB1 mismatching has been associated with a higher risk of acute graft-versus-host disease (aGvHD) and a decreased risk of relapse. A detrimental role of additional HLA-DQB1, HLA-DPB1 and HLA-DRB3/4/5 mismatches (MM) has been recently identified on OS but only in 7/8 HLA-A, -B, -C, and -DRB1 loci URDs HSCT. We investigated the impact of HLA-DPB1 and HLA-DRB3/4/5 MM on outcomes in a large cohort of 10/10 matched URD HSCTs.
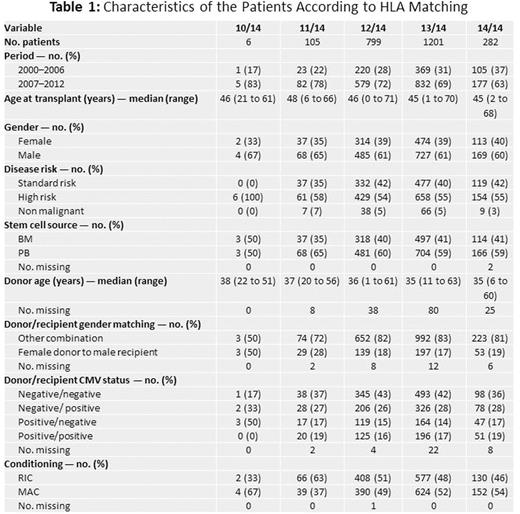
Patients and methods: 2,393 pts who received an initial HSCT from a 10/10 matched URD in 35 French centers were included between January 2000 and October 2012. Informed consent was obtained in accordance with the Declaration of Helsinki. High-resolution typing was performed for HLA-A, -B, -C, -DRB1, -DQB1, -DPB1 and -DRB3/4/5 loci for all donor/recipient pairs. Clinical data were obtained through ProMISe (Project Manager Internet Server), an internet-based system shared by all French transplantation centers. Impact of HLA-DRB3/4/5 and -DPB1 MM was quantitatively and qualitatively evaluated. For quantitative evaluation, patients were classified into 5 different groups according to their global matching level for the 7 considered loci (14/14, 13/14, 12/14, 11/14, 10/14). For qualitative evaluation, MM type and directionality (GvH and host versus graft (HvG) directions) were evaluated. HLA-DPB1 MM were classified as permissive or non-permissive (K Fleischhauer, Lancet Oncol. 2012). The primary composite endpoint for the analysis was GvHD-free and relapse-free survival (GRFS). We defined early GRFS as being alive at 3 months after HSCT with no previous grade III-IV aGvHD and no relapse and late GRFS as being alive >3 months with no previous grade III-IV aGvH, no relapse and no moderate or severe chronic GvHD (cGvHD). Late GRFS was evaluated at months 6, 12, 24 and 36 after HSCT. Acute GvHD, cGvHD, relapse and OS were also studied. Models were adjusted for HSCT period, disease risk, age, sex matching, stem cell source, and conditioning regimen.
Results: Table 1showspopulation characteristics and distribution of cumulative MM. The median follow-up was 59 months. Compared to 14/14 pairs, quantitative evaluation showed a significantly lower early GRFS for pts who received a 10-11/14 (Hazard Ratio HR 2.0, 95% CI 1.4 to 2.9, p=0.0003) or a 12/14 URD HSCT (HR 1.4, 95% CI 1.1 to 1.8, p=0.01). This was related to a significantly increased risk of grade III-IV aGVHD associated with 10-11/14 (HR 2.3, 95% CI 1.5 to 3.7, p=0.0004) and 12/14 pairs (HR 1.7, 95% CI 1.2 to 2.4, p=0.003). 10-11/14 pairs were also associated with a higher risk of death at 3 months (HR 2, 95% CI 1.1 to 3.6, p=0.024). Qualitatively, in pts matched for HLA-DRB3/4/5 but MM for HLA-DPB1 (n=1846, 77.1%), 2 HLA-DPB1 MM and non-permissive HLA-DPB1 MM were associated with a lower early GRFS (HR 1.4, 95% CI 1.1 to 1.9, p=0.01 and HR 1.3, 95% CI 1.0 to 1.7, p=0.02 respectively) due to an increased risk of aGvHD (HR 1.7, 95% CI 1.2 to 2.5, p=0.002 and HR 1.50, 95% CI 1.08 to 2.08, p= 0.017 respectively). Outcomes were not influenced by either GvHD or HvG mismatch directions. Late GRFS analyses once adjusted were not significantly different according to MM numbers, type and directions. Only 19 pairs (0.8%) were DPB1 matched and DRB3/4/5 mismatched (high linkage disequilibrium between DRB3/4/5 and DRB1); HLA-DRB3/4/5 MM could thus not be qualitatively analyzed.
Conclusion: MultipleHLA-DPB1 and HLA-DRB3/4/5 MM have an early impact after 10/10 matched URDs HSCT. The best outcomes are seen in 13 and 14/14 pairs. Early GRFS is significantly impacted by 10-11/14, 12/14, 2 DPB1 MM as well as non-permissive HLA-DPB1 MM URD HSCT which is related to an increased risk of grade III-IV aGvHD. There is a significantly increased risk of mortality for 10-11/14 pairs at 3 months. Prospective evaluation of matching for HLA-DPB1 and HLA-DRB3/4/5 is warranted to reduce early post-HSCT toxicity in donor-recipient 10/10 matched pairs.
Michallet:Bristol-Myers Squibb: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Astellas Pharma: Consultancy, Honoraria; MSD: Consultancy, Honoraria; Genzyme: Consultancy, Honoraria. Peffault De Latour:Pfizer: Consultancy, Honoraria, Research Funding; Alexion: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.