Abstract
Background:
There are a limited number of studies that have evaluated the proteome of MDS patients (pts). Two chemokines (CXCL-4 and CXCL-7) were found to be differentially depressed in patients with MDS compared to patients with other hematologic disorders (Aviado et al, Proc Nat Acad Sci 2007). One study found that normal levels of these proteins are essential for stem cell quiescence, and with their depletion stem cell exhaustion ensues (Bruns I et al, Nat Med). In the current study, we sought to confirm the MDS-specific reduction of these chemokines, and in an exploratory fashion examine the association of CXCL4/CXCL7 pre-HCT plasma levels with MDS disease status pre-HCT and subsequent post HCT outcomes.
Methods:
We analyzed three cohorts of pts >18 years of age reported to CIBMTR from 2008-2011: MDS cohort (N= 80); Non-MDS cohort undergoing allogeneic HCT for either aplastic anemia or non-Hodgkin lymphoma (N= 70); and Normal donors (ND) (N= 79). The primary objectives were to compare the pre-HCT plasma levels of the two chemokines (CXCL-4 and CXCL-7) among the three cohorts, and to explore whether these chemokines correlate with post-HCT disease free survival (DFS), overall survival (OS), relapse and non-relapse mortality (NRM) in the MDS cohort. Abcam's Human ELISA kits were used to measure pre-HCT serum CXCL4 and CXCL7 concentrations. Optimal cut-off points to classify patients as "high" vs. "low" were identified using maximum likelihood method. We also examined whether the use of hypomethylating agents (HMA) pre-HCT correlated with chemokine levels pre-HCT in the MDS cohort.
Results:
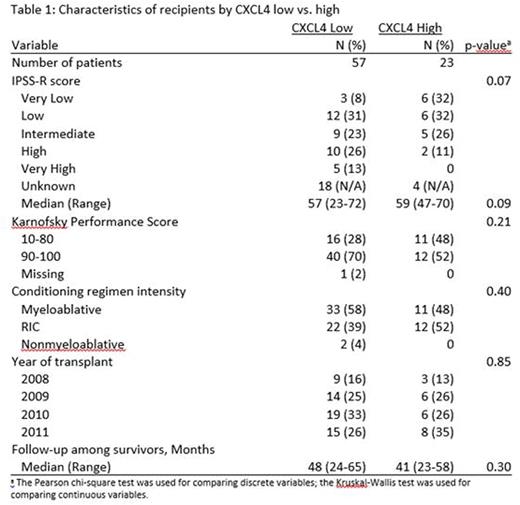
Median ages were 58 yrs, 47 yrs, and 30 yrs for MDS, non-MDS, and ND, respectively. Forty-five pts (56%) in the MDS cohort had advanced stage disease at transplant and 46% had poor or very poor risk cytogenetics based on the International Prognostic Scoring System-Revised (IPSS-R) criteria. Fifty pts (63%) were male and 65% had Karnofsky performance score of 90-100 in MDS cohort. Myeloablative regimen was used in 55% of MDS pts compared to 23% in non-MDS cases. Low CXCL4 levels were seen in 57 (71%) MDS vs. 38 (48%) ND vs. 69 (99%) non-MDS pts (P<0.001) (Fig A). Low CXCL7 levels were seen in 63 (79%) MDS, 47 (59%) ND and 65 (93%) non-MDS pts (p<0.001) (Fig B). In MDS pts with low CXCL4 levels, 39% had high or very high IPSS-R score compared to only 11% among those with high CXCL4 levels (p=0.07) (Table 2). Similarly, among MDS pts with low CXCL7, 36% had high or very high IPSS-R score compared to only 7% among those with high CXCL7 levels (p=0.18) (Table 2). There was no correlation between the use of HMA pre-HCT and the pre-HCT chemokine levels in MDS pts. For MDS pts >50 yrs, there was no correlation between age and CXCL4 and CXCL7 levels. In univariate analysis, neither chemokine was associated with post-HCT OS, DFS, NRM or relapse in MDS pts.
Conclusions:
Our study confirms that levels of chemokines CXCL-4 and CXCL-7 in MDS pts were significantly lower compared to ND. However, in contrast to previous findings by Aivado et al.2007, we did not observe MDS specific reduction as these chemokines were significantly lower among those with NHL and AA compared to MDS patients at HCT. Consistent with previous findings by Aivado et al. we observed a trend towards further reduction of these chemokines among MDS patients with more advanced disease (defined by higher IPSS-R scores) compared to MDS pts with less advanced disease. In our exploratory analysis, we did not observe an association between pre-HCT chemokines levels and post-HCT outcomes among MDS patients. Similarly, the use of HMA among MDS pts was not associated with pre-HCT chemokines levels. An important caveat to this conclusion is that we did not have data on the duration of HMA use. In MDS pts who were >50 yrs, there was no correlation between age and chemokine levels. Large-scale prospective studies are needed to understand more fully the prognostic role of the MDS proteome as well as the complex interplay between proteomic perturbations and acquired somatic mutations these patients often display in determining outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.