Abstract
Introduction: Thrombotic microangiopathies (TMAs) are a group of life-threatening disorders characterized with Coombs negative microangiopathic hemolytic anemia (MAHA), thrombocytopenia and variable degrees of tissue injury associated with microvascular thrombosis. According to underlying pathophysiological mechanisms and treatment approaches TMAs can be sub-classified as thrombotic thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), atypical HUS (aHUS) and secondary TMAs. Here we report the retrospective experience of ThREG (Turkish Hematology Research and Education Group) in patients who were diagnosed with TMA and received therapeutic plasma exchange (TPE).
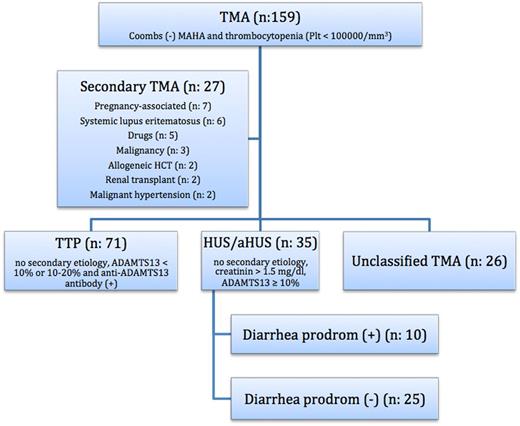
Methods: All consecutive patients who were diagnosed with TMA in last 5 years and treated with TPE by participating centers were included. In order to have a more reliable classification of TMAs, patients without available ADAMTS13 activity at diagnosis were excluded. In all patients serum samples were send for ADAMTS13 activity and anti-ADAMTS13 antibody assays before of TPE. Patients without a secondary etiology of TMA, who had an ADAMTS13 activity < 10% or 10-20% with anti-ADAMTS13 antibodies were diagnosed as TTP. Cases with a known clinical condition associated with TMA were classified as secondary TMA. Patients presenting with renal failure (creatinin > 1.5 mg/dl) who did not belong to TTP or secondary TMA groups, were regarded as HUS/aHUS. All other patients were defined as unclassified TMA. Responses to TPE were evaluated using established criteria defined for TTP. All the data were extracted from medical records of patients.
Results: A total of 159 patients (104 females and 54 males) from 19 centers were included. The median age of the study cohort was 36 (14-84). 71 (44.7%), 35 (22%), 27 (17%) and 26 (16.3%) patients were diagnosed as TTP, HUS/aHUS, secondary TMA and unclassified TMA, respectively (Figure-1). 10 of the patients in HUS/aHUS had a diarrhea prodrome. At presentation 77 (48.4%), 100 (62.9%) and 80 (50.3%) patients had fever, neurological abnormalities and renal failure, respectively. 32 (20.1%) patients had classic pentad of TMAs, namely MAHA, thrombocytopenia, renal failure, neurological abnormalities and fever. Patients received median 17 (1-75) plasma volume exchanges for 14 (1-74) days. 85 (53.5%) cases received concomitant steroid therapy with TPE. Treatment responses could be evaluated in 143 patients. 91 patients (63.6%) responded to TPE, while 51 (36.4%) patients had refractory disease. 20 (14%) refractory patients died during follow-up. 32 TPE-refractory patients who were still alive received following treatments: eculizumab (n: 10), increased TPE intensity alone (n: 7), increased TPE intensity plus steroids (n: 9), rituximab (n: 3) and treatment of underlying malignancy (n: 3).
Discussion: Most patients presenting with TMAs receive TPE as first line treatment. But distinguishing different types of TMAs is of utmost importance, because treatment should be directed according to underlying pathophysiology. Reliable classification of TMAs in daily practice is problematic and sometimes impossible because of the following reasons: 1. Evidence of secondary TMA may not be evident at diagnosis. 2. Evaluation of mutations of complement system regulators/activators for diagnosis of aHUS and stool culture for STEC-associated HUS are mostly unavailable to community practice. As we were unable to do specific stool cultures, 10 patients with diarrhea prodrome were not regarded as HUS instead put into HUS/aHUS group.
Conclusion: As the treatment of various subtypes of TMAs is quite different, we need more powerful and easily accessible tools for differentiation. Until that time, patient presenting with renal failure, no known secondary etiology, and ADAMTS13 activity > 10% should be regarded as aHUS especially if they are unresponsive to first line TPE. In order to plan future treatment strategy, rigorous evaluation for secondary causes of TMAs and evaluation of gene mutations of complement system should follow.
Distribution of TMAs
Demirkan:Amgen: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.