Abstract
Background: Increasing prevalence of diabetes and obesity has registered a simultaneous increase in chronic wounds and defects in tissue repair. Recently PRP was described to be used in the treatment of chronic ulcers. PRP contains cytokines, chemokines and growth factors (GF) derived from platelets which induce molecular and cell mechanisms of natural wound healing. The possible use of GF derived from platelets, and the potential to prolong the shelf life of platelet concentrates, freeze-drying becomes one particularly suitable method to improve wound healing treatment. The use of lyophilized PRP appears to be interesting for greater convenience: only one blood collection, after hydration its soon ready for use, and also due to the highest concentration of bioactive molecules. This study aims to compare intra-lesional freeze-dried and fresh PRP for treatment of acute wound in a pre-clinic model.
Methods: Fresh and freeze-dried PRP was prepared from two human platelet concentrate bags using double spin method. PRP characterization included platelet number and quantification of PDGF-AA, EGF, VEGF and TGF-β1 by Luminex (Millipore). Animal wound model was performed after shaving the dorsum of the rat, and a full-thickness excisional wound (1 cm2) was made to the level of the panniculus carnosus muscle. Thirty animals were divided according to the type o treatment in 3 groups: Fresh PRP (n=10), Freeze-dried PRP (FD-PRP) (n=10) and control saline (n=10). The animals received one perilesional application of 500 µL in the day of wound induction. The monitoring of wound closure was made through macroscopical analysis of wound size in days 3, 7 and 10 after wounding. Animals were sacrificed in the tenth day and the skin was removed for histology with hematoxilin-eosin and Masson´s Trichrome, and immunohistochemistry with α-actin smooth muscle for myofibroblasts and blood vessels, and quantified through image J.
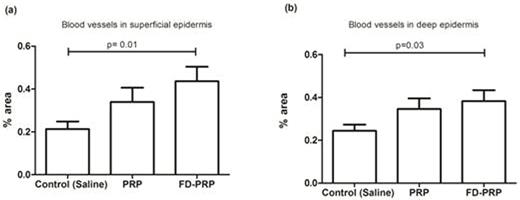
Results: The platelet number of PRP was 5714 x 103 cells / µL, presenting a high platelet recovery. The FD-PRP presented higher level of all GF when compared to fresh PRP from 1.64 to 3.72 folds. The application of PRP or FD-PRP did not induce significantly changes in wound healing kinetics compared to control during all evaluated days. The mean and standard deviation (SD) of area in D3 was 112.9 ± 16.6%, 107.9 ± 21.3 and 100.8 ± 30.2 for control, PRP and FD-PRP, respectively. In D7 it was 54.3 ± 28.9, 63.9 ± 22.8 and 61.6 ± 20.6 for control, PRP and FD-PRP, respectively. In D10 it was 9.9 ± 6.1, 13.9 ± 11.2, 7.7 ± 6.0 for control, PRP and FD-PRP, respectively. In immunohistochemistry of deep epidermis FD-PRP presented a significantly higher concentration of myofibroblasts in comparison with fresh PRP (16.61 ± 9.04 vs. 13.99 ± 14.07, p=0.0095). A significantly higher number of blood vessels was observed in the group treated with FD-PRP (in percentage of area) in comparison to the controls, both in superficial and deep regions of epidermis (0.43 ± 0.5 vs. 0.21 ± 0.22, P=0.01; 0.38 ± 0.44 vs. 0.24 ± 0.25, P=0.03, respectively).
Discussion and conclusion: The most interesting result of this study was the increased number of blood vessels. VEGF plays a central role in promoting angiogenesis during wound repair. Previous studies demonstrated accelerated wound closure with collagen-binding VEGF topical treatment. However, the use of one growth factor has limited success and heterogeneity of clinical results, probably due to the need of multiple bioactive molecules that are necessary in the cascade of complexes events of healing. The use of multiples factors necessary to healing can orchestrated the physiological events resulting in chemotaxis, proliferation and differentiation of cells and the angiogenic process. The use of FD-PRP in this study of acute model of wounds showed positive results, especially in angiogenesis. The practicality and the improve in the shelf life of PRP have a great value in clinical practice and becomes very attractive, showing low cost, the possibility to increase the concentration of GF, various samples ready-to-use and a single blood collection. The investigation of FD-PRP in other clinical situations in which fresh PRP have been used is an interesting approach to be to evaluated to determine its effectiveness.
Quantification of blood vessels through imunohistochemistry using smooth α-actin and treated by Image J software; A) Superficial epidermis; B) Deep epidermis.
Quantification of blood vessels through imunohistochemistry using smooth α-actin and treated by Image J software; A) Superficial epidermis; B) Deep epidermis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.