Abstract
Introduction: PNH is an orphan clonal hematopoietic stem cell disorder characterized by intravascular hemolysis, cytopenias and TE. TE is the leading cause of death in the natural course of PNH. The data on epidemiology, clinical characteristics and outcomes of TE are limited to a few studies and not available in the Russian population of patients with PNH.
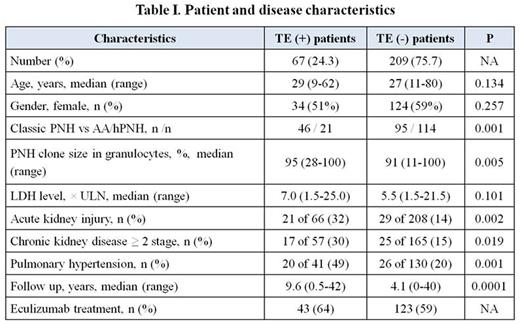
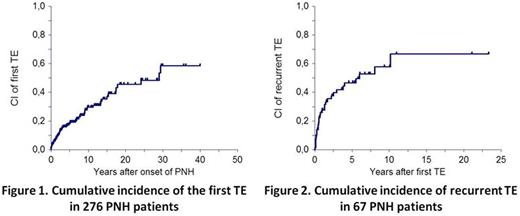
Methods: We conducted a retrospective and prospective analysis of TE in a large cohort of patients with classic PNH and hemolytic PNH associated with aplastic anemia (AA/PNH) in one reference center in Russia. Hemolytic PNH was defined as a granulocyte clone size ≥ 10% and lactate dehydrogenase (LDH) level ≥ 1.5 of upper limit of normal (ULN). The analysis included only the documented episodes of symptomatic TE. Cases of subclinical thrombosis detected using sensitive methods were not considered. Cumulative incidence of TE was calculated using unrelated to TE death and allogeneic HSCT as competing risks. Patients without TE were censored at the last follow-up or date of first treatment with eculizumab.
Results: A total of 276 patients with classic PNH (n=141) and hPNH associated with aplastic anemia (n=135) were included in analysis between 1996 and 2016 (Table 1).
Sixty seven patients (24.3%) developed a total of 118 TE (median, 1; range, 1-7) with the median time between PNH onset and first TE of 2.7 years (range, 0-29). Cumulative incidence of first TE reached 29.7% and 45.5% at 10 and 20 years respectively (Fig. 1). Recurrent TEs were documented in 30 of 67 patients (45%) with the cumulative incidence of second TE of 27.7% and 46.7% at 1 and 5 years respectively (Fig. 2). The median time between the initial TE and the first recurrence was 0.74 years (range, 0.05-10). Routine secondary anticoagulant prophylaxis carried out in 34 patients had no significant impact on 5-year cumulative incidence of recurrent TE (43% vs 50%, p=0.919).
The proportion of TE(+) patients was significantly higher in the classical PNH compared to AA / PNH, but taking into account the duration of the disease, these differences were not found in the cumulative incidence analysis.
TE occurred in venous (64% of patients), arterial (22%) and both venous and arterial sites (14%). The most common sites of venous TE were intra-abdominal veins (n=26, 22%), deep veins (n=22, 18.6%), superficial veins (n=16, 13.5%), pulmonary embolism (n=15, 12.7%) and cerebral veins (n=5, 4.2%). Arterial TE included TIA/ischemic stroke (n=23, 19.5%) and myocardial infarction (n=7, 5.9%).
Patients with TE were also characterized by 2-fold increase in the incidence of acute kidney injury (AKIN) episodes, the presence of chronic kidney disease (CKD) ≥ 2 stage and pulmonary hypertension.
Seventeen of 67 (25%) TE(+) patients died which resulted in 10-year overall survival of 66% (CI 95%, 51-82). The mortality rate was highest in eculizumab naïve cohort: 11 of 24 (46%) patients died and all deaths were directly caused by TEs. In contrast, among the 43 patients with a history of TE treated with eculizumab there was only one death related to the consequences of TE, but 5 patients died due to neutropenic infections (2), solid tumor (1), MDS/AML (1) and complications after HSCT (1).
Conclusions: These data confirm the high incidence and poor prognosis of symptomatic TE in patients with natural history of PNH. TE are often associated with organ dysfunction (AKIN, CKD, pulmonary hypertension), and characterize the highest burden of disease. Early targeted control of intravascular hemolysis is required in all cases at high risk or history of TE in PNH.
Kulagin:Alexion: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.