Abstract
Introduction: Outcomes are poor among Chinese adults with r/r ALL. Current recommendations in China for the treatment of adults with Ph- ALL include induction therapy with vincristine or vindesine, anthracyclines/anthraquinones, and corticosteroids; intensive consolidation therapy following complete remission (CR); and hematopoietic stem cell transplantation (HSCT). Currently, there is a lack of studies assessing treatment status and outcomes in Chinese adults with r/r ALL. The objective of this study was to assess the efficacy of currently available treatments for adults with r/r Ph- ALL in China.
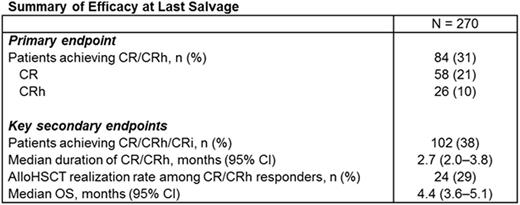
Methods: Between January 2009 and December 2014, adults with r/r B-precursor ALL and defined Philadelphia chromosome status were identified and enrolled from 14 hematology centers in China. All patients were ≥ 15 years of age at time of de novo (initial) diagnosis of ALL, had no central nervous system involvement at time of relapse, and had no isolated extramedullary relapse. Clinical data were retrospectively collected by chart review. The primary analysis set included only patients with r/r Ph- ALL, defined as meeting 1 of the following criteria: primary refractory, had relapsed within 12 months of first CR, relapsed after first or later salvage, or relapsed within 12 months of HSCT. The primary endpoint was rate of overall response (CR or CR with partial hematologic recovery [CRh]) after last salvage treatment. Key secondary endpoints included rate of CR with incomplete hematologic recovery (CR/CRh/CRi), duration of CR/CRh, rate of allogeneic hematopoietic stem cell transplantation (alloHSCT) realization after CR/CRh, and overall survival (OS).
Results: Of 458 eligible patients, 304 (66%) had Ph- ALL, 270 (89%) of whom were in the primary analysis set (female, 46%; median [range] age at diagnosis, 29 (15-73) years). Of these, 45 (17%) had primary refractory disease, 159 (59%) had relapsed within 12 months of first CR, 49 (18%) had relapsed twice or more, and 17 (6%) had relapsed within 12 months post-HSCT. Baseline characteristics at the time of last salvage therapy among patients without prior HSCT included 195 (72%) with no prior salvage, 45 (17%) with 1 prior salvage, and 6 (2%) with ≥ 2 prior salvage treatments. Prior HSCT (n = 24; 9%) included both autologous (n = 8) and allogeneic (n = 16). Among those with prior HSCT, 18 (7%) had prior salvage, 6 (2%) had 1 prior salvage, and none had ≥ 2 prior salvages.
Efficacy data at last salvage are presented in the table. Overall, 31% (84/270; 95% confidence interval [CI], 26%-37%) of patients achieved CR/CRh at last salvage. The median time to CR/CRh was 30 days. Median (range) number of therapies to CR/CRh was 1 (1-3). The occurrence of CR/CRh by line of salvage was 104/254 (41%) for 1st line, 13/55 (24%) for 2nd line, and 1/6 (17%) for 3rd line or later. Median (95% CI) duration of CR/CRh at last salvage was 2.7 (2.0-3.8) months with 57% events among 84 patients who achieved CR/CRh. Among CR/CRh responders, 13 of 16 evaluable patients (81%) achieved a minimal residual disease response. Median (95% CI) OS was 4.4 (3.6-5.1) months, with 54 (20%) deaths among 270 patients. At last salvage, 24/84 (29%) responders subsequently received alloHSCT.
Conclusions: In this population of Chinese adults with r/r Ph- ALL treated with currently available salvage chemotherapies, CR/CRh responses were low (31%) and prognosis was poor. The median duration of CR/CRh was short (2.7 months), and the alloHSCT realization rate was low among responders. Thus, new therapies are needed to improve treatment outcomes in Chinese adults with primary refractory or relapsed Ph- ALL.
Meng:Amgen: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.