Abstract
Introduction. A recent study showed that receiving a hematopoietic cell transplant (HCT) from donors with long leukocyte relative telomere length (RTL) was associated with improved survival in patients with severe aplastic anemia who primarily received bone marrow grafts at age <40 years. Here, we tested the effect of donor RTL on post-HCT outcomes in a large cohort of patients with acute leukemia.
Methods. From the Center for International Blood and Marrow Transplant Research (CIBMTR®) database, we identified 1,097 patients who received unrelated HCT for acute myeloid leukemia (AML) or acute lymphocytic leukemia (ALL) and fulfilled the following criteria: 1) HCT between 2004 and 2012, 2) available pre-HCT blood sample for the donor, 3) 8/8 HLA matching, and 3) myeloablative conditioning. We used qPCR to measure RTL; 1084 samples completed testing (597 measured at Telomere Diagnostics, Inc. and 487 at the Cancer Genomics Research Laboratory, NCI). Telomere Diagnostics samples were randomly divided into discovery (n=300) and validation (n=297) cohorts; the NCI samples served as a 2nd validation cohort (N=500). Cox proportional hazard models were used for statistical analyses. All analyses were adjusted for donor age together with clinical factors that met statistical inclusion criteria in a multivariate model. Donor RTL was categorized into short (≤25th percentile based on cohort-specific distribution), or long otherwise. Follow-up ended in November 2014.
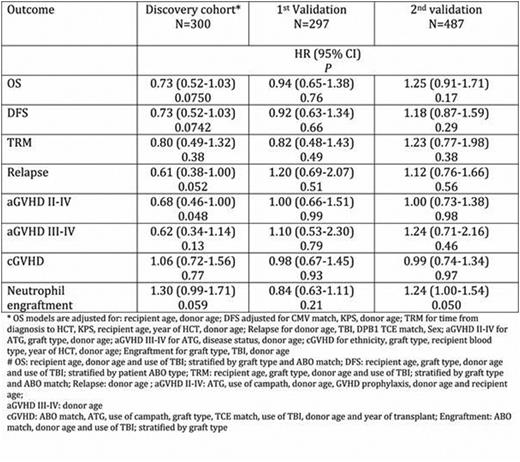
Results. All patient demographics, disease- and HCT-related characteristics were similar in the discovery, 1st, and 2nd validation cohorts with the exception of graft source (peripheral blood stem cells in 67%, 60%, and 70%, respectively, p=0.008), and year of HCT (0%, 0%, and 37% between 2008-2012, respectively, p<0.001). Results from the discovery cohort suggested that long donor RTL may be associated with: 1) improved overall survival (HR=0.73, 95% CI=0.52-1.03, p=0.08), and disease-free survival (HR=0.73, 95% CI=0.52-1.03, p=0.07); 2) higher probability of neutrophil engraftment (HR=1.3, 95% CI=0.99-1.71, p=0.06), and 3) decreased risk of relapse (HR=0.61, 95% CI=0.38-1.00, p=0.05) and acute graft-versus-host disease II-IV (HR=0.68, 95% CI=0.46-1.0, p=0.05). However, none of these results were replicated in the two validation cohorts with the exception of a higher probability of neutrophil engraftment observed in the 2nd (HR=1.24, 95% CI=1.0-1.54, p=0.05), but not the 1st validation (HR=0.84, 95% CI=0.63-1.11, p=0.21). All three cohorts were combined for a final exploratory analysis and no associations (all p>0.3) were found between donor telomere length and any outcomes.
Conclusions. Donor telomere length is not associated with outcomes in unrelated donor HCT for patients with acute leukemia.
Impact of donor RTL comparing the three longest quartiles to the shortest quartile.
Impact of donor RTL comparing the three longest quartiles to the shortest quartile.
Loftus:Telomere Diagnostics, Inc.: Consultancy. Friedman:Telomere Diagnostics, Inc.: Consultancy. Buturovic:Clinical Persona: Consultancy. Blauwkamp:Telomere Diagnostics, Inc.: Employment. Shelton:Telomere Diagnostics, Inc.: Employment.
Author notes
Asterisk with author names denotes non-ASH members.