Abstract
Background: Recent data showed that gamma delta T cells can act as a vast functional setting of immune defense against tumors. Our previous study found that persist clonally expanded TRDV4 T cells might be relatively to better outcome for the patient with T-cell acute lymphoblastic leukemia (T-ALL) after hematopoietic stem cell transplantation (HSCT). However, little is known, the distribution and clonality of TRDV repertoire of gamma delta T cells in peripheral blood (PB) and its potential effect for clinical outcome in acute myeloid leukemia (AML) patients.
Methods: Gamma delta T cells were sorted from peripheral blood of 30 patients with untreated de novo AML (AML-M0 6 cases, M1 1 case, M2 5 cases, M3 10 cases, M4 3 cases and M5 5 cases) and were observed the distribution of TRDV repertoire, while 12 healthy individuals served as normal controls. Then the TRDV repertoire were further analyzed by Genescan technique to determine the size of complementarity determining region 3 (CDR3) of TRDV (1-8) subfamilies genes and to evaluate the clonality of the detectable subfamilies of gamma delta cells. The binary Logistic regression analysis was used to explore the associations between clonal expansion of gamma delta T cells and outcome of AML patients.
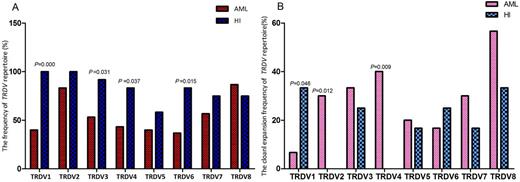
Results: The frequencies of TRDV1, TRDV3, TRDV4 and TRDV6 in gamma delta T cells from AML patients were significantly lower than that from healthy individuals (HI) (Figure A). The most frequently expanded TRDV subfamilies in AML patients were TRDV8 (56.67%) and TRDV4 (40%). Furthermore, the most frequently oligoclonally expanded TRDV subfamilies from AML patients were TRDV2 and TRDV4 subfamilies, and the clonal expansion frequencies were significant higher than that from healthy individuals, however, a significant lower clonal expansion frequency of TRDV1 was observed in AML patients (Figure B). Importantly, oligoclonalities of TRDV4 and TRDV8subfamilies were the independent protective factors for complete remission. In addition, the oligoclonal expansion frequencies of TRDV5 and TRDV6 subfamilies from the recurrence cases were significantly higher than that from non-recurrence cases. Significantly, oligoclonal TRDV5 and TRDV6subfamilies were found in the patients who developed AML relapse in different time point after first complete remission.
Conclusions: The distribution and clonality of TRDV subfamilies significantly changed in gamma delta T cells from AML patients. Clonally expanded TRDV4 and TRDV8 T cells might contribute to immune response against AML, while oligoclonal TRDV5 and TRDV6 may be accompanied to patients who underwent AML relapse, the function of such oligoclones of gamma delta T cells is needed further investigation. Overall, these TRDV gamma delta T cell clones might be a potential immune biomarker for AML outcome.
Foundation: This study was supported by grants from Natural Science Foundation of China (No.81200388), Natural Science Foundation of Guangdong Province (NO.2014A030313380) and the Project of the Zhujiang Science & Technology Star of Guangzhou City (No. 2013J2200046).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.