Abstract
Background
Approximately 15% of children newly diagnosed for acute lymphoblastic leukemia (ALL) present with the T cell lineage (T-ALL), which historically has had inferior outcomes compared to the children with precursor-B cell ALL. In this study, we analyzed the efficacy of the Chinese Children Leukemia Group 2008 (CCLG-ALL 2008) protocol on pediatric T-ALL patients enrolled from 4 centers located at north, east, and southwest of China, to identify specific prognostic factors.
Patients and methods
Patients enrolled on the CCLG-ALL 2008 Protocol came from four hospitals in China: two hospitals in the southwest, one in the east, and one in the north, with 33, 37, 34 and 48 patients respectively. The study was approved by the hospitals' Ethical Committee, with informed consent obtained from patients' patents or legal guardians.
Definitions: Failures of relapse-free survival (RFS) included relapse and death of any cause. M1: Blast <5%, M2: 5%≤Blast ≤25%, M3: Blast >25%.
Results
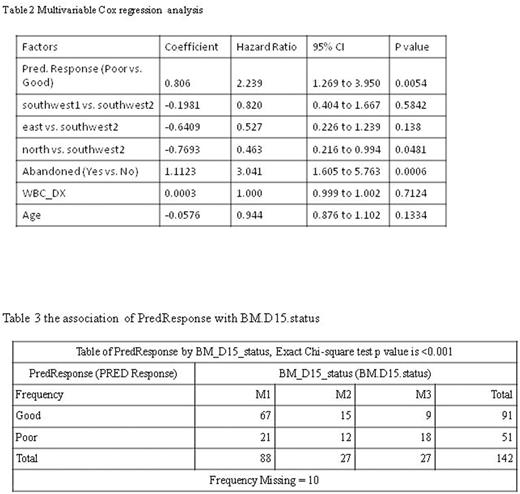
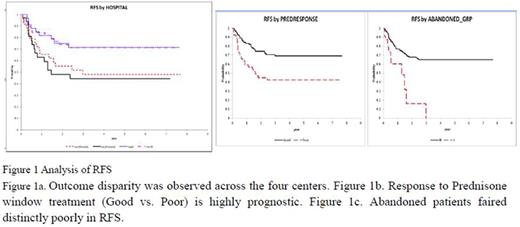
Outcome disparity is observed across the four hospitals (Table 1 and Figure 1). Response to prednisone window treatment (Good vs. Poor) was highly prognostic and its prognostic value held universally across the centers despite the outcome disparity across the centers and abandonment: log-rank test stratified by centers (hospitals) P value = 0.0311, and by abandonment (Y vs. N) P = 0.0004. Multivariable Cox regression analysis showed that response to prednisone window treatment was an independent early (before end of remission induction) prognostic factor (Table 2). The hazard ratio of prednisone response (Poor vs. Good) was 2.6 (95% CI 1.49 to 4.57) after accounting for RFS disparities across centers and abandonment. When further adjusted for post-induction prognostic markers by Day-35 and Month-three bone marrow status (M1, M2 or M3), response to predisone window remained boarder-line significant (P=0.0683). Prednisone response was only significantly associated with Day-15 bone-marrow status, with poor responders tended to likely have M2 and M3 marrow status at Day 15 (Table 3). Day-15 and Day-35 marrow status was not significantly associated with RFS, but patients with Day-35 M2 and M3 status tended to fail early. Marrow status before intensification (Month 3) seemed highly associated with RFS, with all 4 M3 patients failed within 1 year.
The percentage of abandonment in the southwest 1, the southwest 2, the east, and the north hospital was 21.6%, 33.3%, 8.8% and 25% respectively; the difference was not significant (P=0.1078). Nonetheless the east hospital seemed to have distinctly lower percentage of abandonment. The percentage of non-urban patients in the southwest1, the southwest2, the east and the north is 52.8%, 75.8%, 61.8% and 68.8% respectively; this difference was not significant (P=0.2171), although the percentage seemed higher in southwest. Patients from urban area tended to fair better in RFS but the difference was not statistically significant (P=0.1785). There was a weak trend that abandonment rate tended to be higher among non-urban patients, but not statistically significant (P=0.3361). Patients' Day-35 bone marrow status (with M2 and M3 marrow related to higher likelihood of abandonment), abandonment and socio-economic status might be relevant factors for the inter-center disparity in RFS. With the current data however, we are unable to identify any strong factor that can explain the inter-center disparity of treatment outcome.
Conclusion
Response to prednisone window treatment is a universal early prognostic marker in Chinese children with T lineage ALL despite outcome disparity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.