Abstract
Background: MYC protein is expressed in 30-50% of diffuse large B cell lymphoma (DLBCL) and is associated with concomitant expression of BCL2 in 20% to 35% of cases. DLBCLs with co-expression of MYC and BCL2 are called double-expressor lymphomas (DELs); whereas double-hit lymphomas (DHLs) have MYC and BCL2 or BCL6 rearrangement as detected by fluorescence in situ hybridization (FISH) or standard cytogenetics and are currently classified by the World Health Organization as high grade B cell lymphoma (HGBL). MYC/BCL2 double expression is an independent risk factor of DLBCL relapse or progression. In several studies, DELs were shown to have worse outcomes than other DLBCLs, but not as much aggressiveness as the DHLs (HGBL). Poor response to standard chemotherapy CHOP or R-CHOP is seen with DHLs and DELs with a median overall survival of <12 months. The purpose of this study was to characterize DELs amongst veteran patients with DLBCL and their outcomes.
Methods: This is an IRB-approved, retrospective study of patients diagnosed with DLBCL between 1/1996 and 1/2016 at the Washington DC Veterans Affairs Medical Center. Sixty nine DLBCL patients were identified. All patients with unavailable tissue for pathology testing were excluded. Immunohistochemistry (IHC) stains were reviewed for CD3, CD5, CD10, CD20, CD30, BCL2, BCL6, C-MYC, MUM-1, MIB1, Cyclin-D1, and p53. DELs were defined by concomitant expression of MYC and BCL2 detected by IHC (cutoffs-30% MYC, 40% BCL2). We did not sub-classify our patients into DHLs because of unavailability of MYC and BCL2 rearrangement results by FISH. Demographic and laboratory data at diagnosis, treatment regimens and outcomes in terms of relapse and death were analyzed. Student's t-test was used to compare means and chi-square to compare proportions.
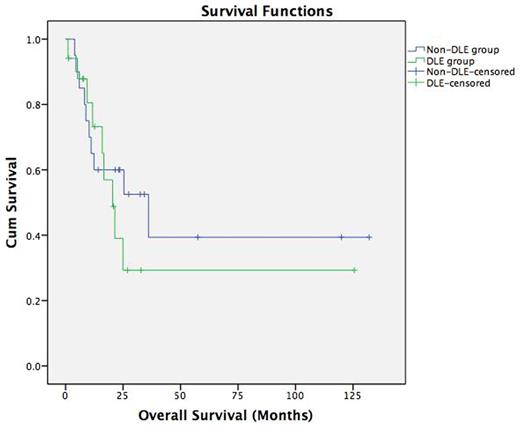
Results: Sixty nine eligible cases of DLBCL were identified, 31 were excluded because of insufficient tissue for full characterization, leaving us with 38 cases for analysis. All cases were CD20 positive with high MIB1. MYC was positive in 19 cases (50%) of whom 17 were as well positive for BCL2 (44.7%) (DELs); the remaining 21 were non-DELs. Median age at diagnosis for all patients was 65 years. Stages at diagnosis for all patients were as follows: I (2 patients; 5.3%), II (8; 21.1%), III (7; 18.4%), IV (20; 52.6%). Stage and presence of extra-nodal disease were not significantly different in the DEL vs the non-DEL groups. The majority of DEL patients had an IPI score of 3 (intermediate-high) compared to a score of 2 (low-intermediate) in non-DEL patients (difference was not significant). Mean LDH at diagnosis for all patients was 365.7 ±273 IU/L (133-1285); higher in DEL (422.9±340.5) as compared to non-DEL (314±182) patients. Within the DEL group, 5 patients (29.4%) received R-CHOP; 11 (64.7%) received R-EPOCH as first line chemotherapy. Four out of the 5 (80%) treated initially with R-CHOP relapsed and eventually died. Of the 11 DEL patients treated with R-EPOCH, 2 (18.2%) relapsed and one of these two died. The relapse rate between the 2 treatment groups of DEL was significantly higher for R-CHOP (p=0.042). Of 21 non-DEL patients, 14 (66.7%) remained in remission; 2((9.5%) relapsed; and 5(23.8%) were lost-to-follow-up. Nineteen (50%) patients died and median overall survival (OS) was 18.5 months for the whole group (20.4 vs 36.1 in the DEL vs non-DEL groups respectively; no statistical significance).
Conclusions: The proportion of DELs identified amongst DLBCL in our study is consistent with the literature. As expected, patients with DEL had a worse OS than non-DEL patients in our study, which is consistent with DEL's poor prognosis. Although the sample size in our study is small, there was a more favorable outcome with R-EPOCH treatment of DEL. Larger prospective and interventional studies are needed to confirm these results, develop new treatment strategies for DEL, and better characterize the underlying biology driving its poor prognosis.
Kaplan-Meier survival curves comparing overall survival in DEL vs non-DEL groups
Kaplan-Meier survival curves comparing overall survival in DEL vs non-DEL groups
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.