Abstract
It is difficult to find figures for the expected rate of early mortality in diffuse large B-cell non-Hodgkin lymphoma (DLBCL) as many of the patients who are destined to die early do not enter clinical trials. Our own rate of early mortality (death within 100 days of the diagnostic test being performed) was higher than we had anticipated (23%). We undertook a study to look at risk factors for early mortality, and to see if there were any factors which could be improved by altering our investigation and initial management.
Our haematology database has baseline demographic and prognostic information on all cases of haematological malignancy diagnosed in our centre. A two year period was chosen retrospectively from 1st January 2013 until 31st December 2014. This gave 97 registered patients with DLBCL.
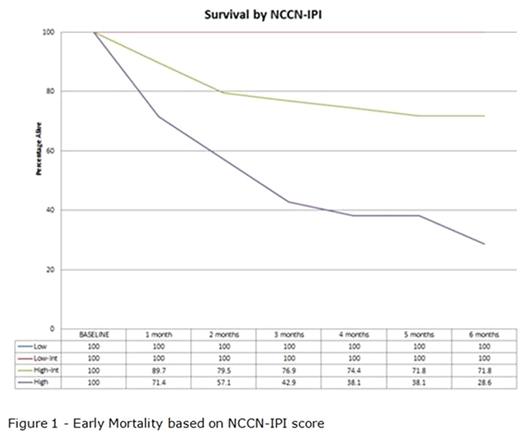
Early mortality was significantly related to the patient age, Eastern Cooperative Oncology Group (ECOG) performance status, lactase dehydrogenase value, presence of 2 or more sites of extranodal disease and the presence of B-symptoms. We did not see a significant relationship to the presence of marrow disease or the presence of disease bulk. As the majority of the relevant factors are already part of validated prognostic scoring systems, we evaluated the (International Prognostic Index) IPI, the R-IPI (revised International Prognostic Index) and the NCCN-IPI (enhanced International Prognostic Index) to see which was the best predictor of early mortality. The IPI gave the chance of 100 day mortality as 4% for low or low-intermediate risk patients, 16% for high-intermediate risk patients and 53% for high risk patients. The R-IPI gave the chance of 100 day mortality as 0% for low risk patients, 5% for intermediate risk patients and 48% for high risk patients. The NCCN-IPI gave the chance of 100 day mortality as 0% for low or low-intermediate risk patients, 13% for high-intermediate risk patients and 57% for high risk patients (figure 1). By six months, the mortality rate in high risk NCCN-IPI patients had reached 71% while the low and low-intermediate groups remained at 0%. Some patients were included who were not considered for potentially curative chemotherapy. Even with these patients excluded, the risk of 100 day mortality was still 50% in the high risk NCCN-IPI group.
Some of the risk factors for mortality will likely worsen if the diagnosis or initial treatment are delayed. We therefore looked at the overall pathway from referral until first treatment. We found that those with early mortality tended to have a shorter time course until receiving their first treatment, likely reflecting the fact that they were more unwell when they first presented.
Maddox:Janssen: Other: Funding to attend ASH 2016 (travel, accommodation, registration); Boehringer-Ingelheim: Other: Funding to attend ASH 2014 (travel, accommodation, registration).
Author notes
Asterisk with author names denotes non-ASH members.