Abstract
Introduction
Patients with hematologic malignancies are at higher risk for infection due to the nature of their immunocompromised status, therapy-related complications, and numerous other factors. Multiple myeloma (MM) is the second most common hematologic malignancy after non-Hodgkin's lymphomas. Current literature on bone and joint infections (BJI) in MM is limited to case reports, and this study aims to identify the frequency and characteristics of BJI in MM.
Methods
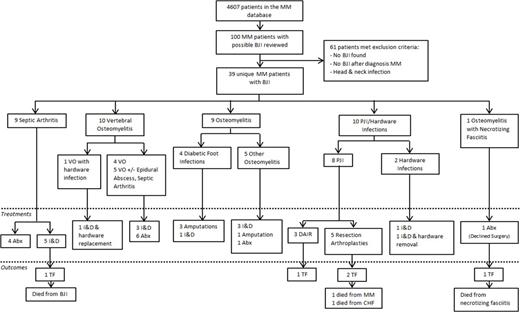
We retrospectively reviewed 4607 patients within the MM database at Mayo Clinic from 1/1/2005 through 1/1/2015. A computerized search of the electronic medical record using diagnosis codes, pathology reports, and free text searches, followed by manual chart review, identified 39 unique patients with BJI as depicted in Figure 1.
Results
Of the 39 patients with BJI and a diagnosis of multiple myeloma, 28/39 (72%) were male, and median age was 70 years-old (range 39-86). 35/39 (90%) had IgG subtype MM, and 21/39 (54%) were in remission from MM while 4/39 (10%) were neutropenic at the time of BJI. 14/39 (36%) occurred after hematopoietic stem cell transplant, and the median duration from transplant to BJI was 45.0 months (range 1.0-88.7). 11/39 (28%) had chronic kidney disease on chart review, and 8/39 (21%) were on corticosteroids. 32/39 (82%) had prior exposure to chemotherapy, and median duration from most recent chemotherapy to BJI was 32 days (range 0-1559).
Septic arthritis (9/39, 23%) and osteomyelitis (9/39, 23%) occurred most frequently followed by prosthetic joint infection (PJI) (8/39, 21%). Pathogens were primarily Gram positive organisms (20/39, 51%), and 7/20 (35%) had polymicrobial infections. All patients received culture-guided induction antimicrobial therapy. 27/39 (69%) underwent surgical intervention. Treatment and outcomes by infection can be seen in Figure 1.
Of the 5 (13%) treatment failures (TF), 3 (60%) had PJI while 1 (20%) had osteomyelitis with necrotizing fasciitis, and 1 (20%) had septic arthritis. Median time from diagnosis of BJI to TF was 6.3 months (range 0.0-13.5), and none of the TF were neutropenic at the time of BJI. 26/39 (67%) were alive one year after BJI, and at latest chart review, 8/39 (21%) were alive, of whom 7 were treated successfully. Median overall survival from diagnosis of BJI was 34.3 months for all cases.
Conclusions
BJI are uncommon in MM, and pathogens are similar to patients without MM, though with polymicrobial infections occurring frequently. Treatment is successful in the majority of cases, but PJI appear to have higher TF rates. However, TF may not necessarily correlate with hematologic status or survival.
Flowchart of the multiple myeloma study cohort, BJI, treatment, and outcomes
MM = Multiple Myeloma; BJI = Bone and Joint Infection; PJI = Prosthetic Joint Infections; VO = Vertebral Osteomyelitis; I&D = Irrigation & Debridement; Abx = Antibiotic Therapy Alone;
DAIR = Debridement and Implant Retention; TF = Treatment Failure; CHF = Congestive Heart Failure
Flowchart of the multiple myeloma study cohort, BJI, treatment, and outcomes
MM = Multiple Myeloma; BJI = Bone and Joint Infection; PJI = Prosthetic Joint Infections; VO = Vertebral Osteomyelitis; I&D = Irrigation & Debridement; Abx = Antibiotic Therapy Alone;
DAIR = Debridement and Implant Retention; TF = Treatment Failure; CHF = Congestive Heart Failure
Kapoor:Amgen: Research Funding; Takeda: Research Funding; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.