Abstract
Introduction: Myelodysplastic syndromes (MDS) comprise a broad spectrum of hematologic malignancies with varying clinical courses; although most deaths are attributed to MDS, many patients will die of other attributable causes, independent of or potentially augmented by their underlying cancer. Cardiovascular (CV) disease is a frequently attributed cause of death in these patients, and may be influenced by CV care patterns in a patient's county of residence. Patients who live in counties with worse CV outcomes may be at greater risk of CV complications and death. We sought to determine whether regional quality of CV care in the US, measured by the rate of CV death in a county, impacts the cumulative incidence of death attributed to CV disease among MDS patients.
Methods: We used the Surveillance, Epidemiology, and End Results (SEER) database from the National Cancer Institute to identify patients, age 15 and older, with a new diagnosis of MDS between 2001 and 2011. We identified 29,571 patients with a known age at diagnosis and follow-up, for whom MDS was the first cancer diagnosed in SEER. We grouped patients into lower risk disease (RA, RT, RN, and RARS), intermediate risk disease (MDS-unclassified, del(5q), RCMD, and t-MDS) and higher risk disease (RAEB and RAEB-T) according to SEER classifications. The incidence of a given cause of death (COD) was estimated by the cumulative incidence method identifying each COD as competing risks using R statistical software, and tested using the Gray test.
We identified population rates of CV-specific mortality, according to the National Center for Health Statistics and available through SEER*Stat, in all counties with at least one MDS diagnosis over the study period. If the rate of death due to cardiovascular disease in a county was below the 25th percentile, then the CV performance was considered "good", if above the 75th percentile then the CV performance was considered "poor", and all others were considered "intermediate." Patients with MDS were grouped into a county CV performance quartile according to the rate of CV death in that county at the time of diagnosis.
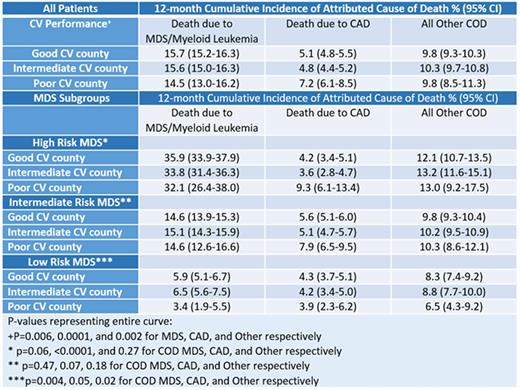
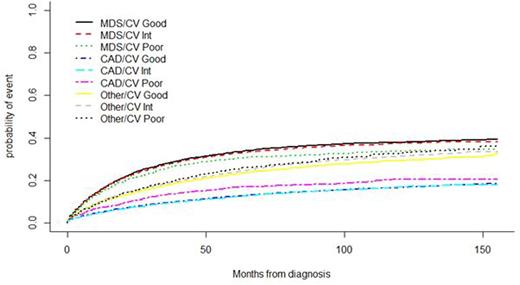
Results: The median age at diagnosis was 76 years (range 15-109) and the patients were 54% male. Patients were divided among lower risk (21%), intermediate risk (66%), and higher risk MDS (13%). Cause of death was reported for 29,344 patients. 602 counties had 1 diagnosis of MDS between 2001 and 2011, 599 of which reported overall CV mortality rates. A total of 15,856 MDS patients (54%) lived in counties with good CV performance (less than or equal to the 25th percentile of CV mortality) during the study period, while 11,845 (40%) lived in counties with intermediate CV performance, and 1817 (6%) lived in poor CV performance counties. MDS patients living in poor CV performance counties had a cumulative incidence of death attributed to cardiovascular disease of 7.2% at 12 months, compared to 4.8% and 5.1% among intermediate and good CV performance counties, respectively (p=0.0001). Death attributed to MDS was 15.7%, 15.6%, and 14.5% at 12 months for patients living in good, intermediate, and poor CV performance counties, respectively (Table 1). When looking specifically at MDS risk groups, it appeared that county CV performance had a greater impact on patients with intermediate and higher risk MDS (Table 1). Patients with higher risk MDS living in poor CV performance counties had a 12-month cumulative incidence of death due to CV disease of 9.3% compared to 4.2% and 3.6% in good and intermediate CV performance counties (p<0.0001), while there was a trend toward fewer deaths due to MDS (p=0.06), and no difference in death attributed to other causes (p=0.27) at 12 months.
Conclusions: Most MDS patients live in counties with good CV performance; MDS patients living in counties with higher cardiovascular mortality have higher rates of death attributed to cardiovascular disease than do MDS patients living in intermediate or low cardiovascular mortality regions, while death attributed to MDS or other causes is relatively stable. This is more apparent among patients with higher risk MDS. These findings suggest that cardiovascular disease may be a modifiable risk factor for MDS patients.
12-Month Cumulative Incidence of Death due to MDS, CAD, and other causes.
12-Month Cumulative Incidence of Death due to MDS, CAD, and other causes.
Cause of Death According to County Cardiovascular Performance.
Cause of Death According to County Cardiovascular Performance.
Hobbs:Incyte: Other: participation in advisory board; Agios: Other: participation in advisory board. Fathi:Seattle Genetics: Consultancy, Other: Advisory Board participation, Research Funding; Bexalata: Other: Advisory Board participation; Celgene: Consultancy, Research Funding; Merck: Other: Advisory Board participation; Agios Pharmaceuticals: Other: Advisory Board participation.
Author notes
Asterisk with author names denotes non-ASH members.