Abstract
Introduction: Chemotherapy-induced cardiotoxicity is an important concern in the long-term survivors era, especially in those younger patients who may suffer excess cardiovascular morbidity and worse outcomes. There is no consensus on monitoring criteria for this phenomenon and prompt therapy has not been yet properly established. We aim to evaluate prospectively early detection of cardiotoxicity, incidence, timing of occurrence and pre-existing factors during two years.
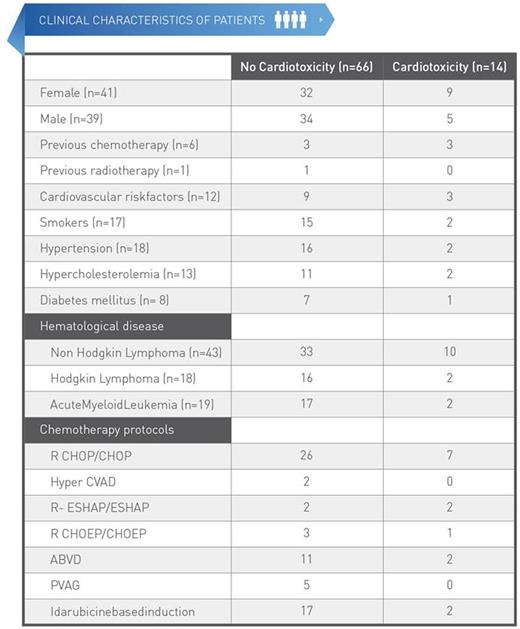
Methods: This prospective study is being conducted at La Paz University Hospital in the period 2012-2013 (n=80) (age 18-84) based on anthracycline chemotherapy. A second phase of the study is ongoing, pending completion of the two year follow-up. Patients' levels of analytical biomarkers cardiac troponin (cTnl) and B type natriuretic peptid (NT pro BNP), echocardiogram parameters left ventricular ejection fraction (LVEF) and global longitudinal strain (GLS) were measured before starting chemotherapy, 3 weeks and 3 months afterwards, and then every six months during 2 years. In the first visit different clinical variables were also measured, including age, sex, body mass index, cardiovascular risk factors and previous treatments with chemotherapy and radiotherapy. Cardiotoxicity was defined as a reduction in LVEF <50% or >10% with basal >50%. Another cardiotoxicity conditions such as ischemic cardiomyopathy, arrhythmia, pericarditis and valvular heart disease were also considered. The cumulative dose of chemotherapy was measured in every visit.
Results: Eighty patients were included; 49% women; 53.75% non-Hodgkin lymphoma, 22.5% Hodgkin lymphoma and 23.75% acute myeloid leukemia. Fifteen patients died (18.75%), 100% due to tumour related causes. Nine patients did not attend follow-up (11.25%). A total of 14 cardiotoxicity events occurred (17.5%): the most frequent event was reduction in LVEF (78,5%). Ischemic events and valvular disease were also observed. No hospitalization was needed in any of the events. Two of them recovered LVEF-levels spontaneously in the next visit. The other 9 were treated with heart failure therapy: 8 with ACE (angiotensin converting enzyme) inhibitors and beta- blockers and 1 with ACE inhibitors. Six (66.6%) of those who received specific treatment recovered basal LVEF-levels, 2 maintained LVEF dysfunction, and 1 died during follow-up due to tumour-related causes. In 85.7% of patients, cardiotoxicity occurred within the first year of follow-up. Basal LVEF and previous treatment with chemotherapy were significant predictors of subsequent cardiotoxicity (Cox regression model).
Conclusions: early detection of cardiotoxic events provides an opportunity to start heart failure therapy on time to prevent progression to established heart failure. Previous chemotherapy treatment points to an increased risk of cardiotoxicity, so more intensive surveillance is necessary. Extended analysis of patients being included in the ongoing study will extend the information about cumulative anthracycline dose and cardiotoxicity induced by non-anthracycline chemotherapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.