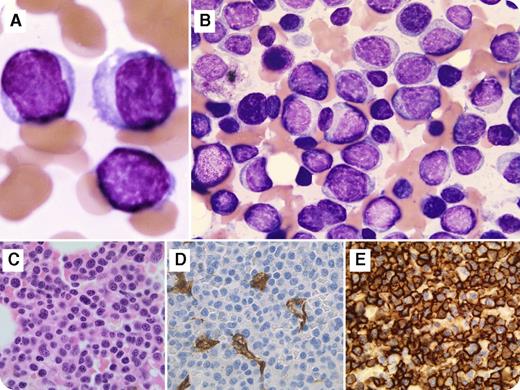
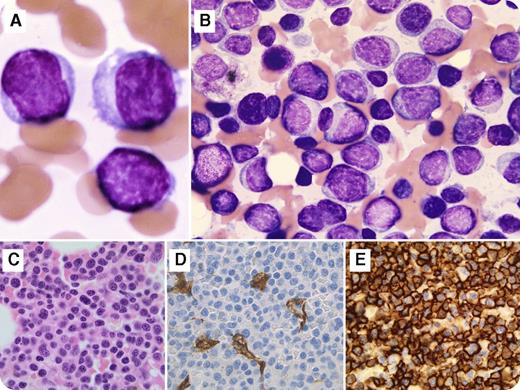
A 63-year-old woman presented with fatigue that increased over 2 months. The blood work showed a white blood cell count of 3.8 × 109/L, hemoglobin of 8.8 g/dL, platelet count of 51 × 109/L, and immunoglobulin G kappa paraproteins. There was no evidence of bone lytic lesions by imaging analysis. A bone marrow aspiration demonstrated diffuse infiltration of mononuclear cells, including the blast-like cells which showed dispersed chromatin, high nuclear-cytoplasmic ratio, and the nucleus concentrically placed with no perinuclear hof (panels A and B; original magnification ×100; May-Grünwald-Giemsa stain). Immunohistochemistry on bone marrow biopsy (panel C; original magnification ×40; hematoxylin and eosin stain) revealed sheets of abnormal cells that were positive for CD138 (panel E; original magnification ×40; CD138 immunostain), MUM1, CD79b, CD117 (dim, partial), and cytoplasmic kappa and were negative for CD34 (panel D; original magnification ×40; CD34 immunostain), TdT, MPO, CD33, CD68, CD56, lysozyme, and CD3. A deletion of chromosome 13q14 was detected by fluorescence in situ hybridization. Overall, the findings were consistent with a plasma cell myeloma with plasmablastic features.
Plasmablastic type is an uncommon aggressive morphologic variant of multiple myeloma with an adverse outcome. This feature is associated with several unfavorable risk parameters, including higher international staging score, more frequent renal insufficiency, extensive bone marrow infiltration, increased plasma cell labeling index, and del(13q). Because myeloma cells can express myelomonocytic markers, and because the blasts of acute myeloid leukemia may express CD56 and CD38, knowing about this morphologic variant is important to distinguish it from acute leukemia.
A 63-year-old woman presented with fatigue that increased over 2 months. The blood work showed a white blood cell count of 3.8 × 109/L, hemoglobin of 8.8 g/dL, platelet count of 51 × 109/L, and immunoglobulin G kappa paraproteins. There was no evidence of bone lytic lesions by imaging analysis. A bone marrow aspiration demonstrated diffuse infiltration of mononuclear cells, including the blast-like cells which showed dispersed chromatin, high nuclear-cytoplasmic ratio, and the nucleus concentrically placed with no perinuclear hof (panels A and B; original magnification ×100; May-Grünwald-Giemsa stain). Immunohistochemistry on bone marrow biopsy (panel C; original magnification ×40; hematoxylin and eosin stain) revealed sheets of abnormal cells that were positive for CD138 (panel E; original magnification ×40; CD138 immunostain), MUM1, CD79b, CD117 (dim, partial), and cytoplasmic kappa and were negative for CD34 (panel D; original magnification ×40; CD34 immunostain), TdT, MPO, CD33, CD68, CD56, lysozyme, and CD3. A deletion of chromosome 13q14 was detected by fluorescence in situ hybridization. Overall, the findings were consistent with a plasma cell myeloma with plasmablastic features.
Plasmablastic type is an uncommon aggressive morphologic variant of multiple myeloma with an adverse outcome. This feature is associated with several unfavorable risk parameters, including higher international staging score, more frequent renal insufficiency, extensive bone marrow infiltration, increased plasma cell labeling index, and del(13q). Because myeloma cells can express myelomonocytic markers, and because the blasts of acute myeloid leukemia may express CD56 and CD38, knowing about this morphologic variant is important to distinguish it from acute leukemia.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.