In this issue of Blood, Desai et al report a large retrospective analysis from the University of Miami including 182 patients with primary ocular adnexal mucosa-associated lymphoid tissue (MALT) lymphoma (orbital marginal zone lymphoma [MZL]).1 Most were at an early stage (82%), and 76% were treated successfully with orbital irradiation. Treatment and follow-up data spanned 31 years. This study reaffirms the excellent long-term control of orbital MZL with localized radiation therapy (RT; complete remission [CR] rate >97%); only 3 deaths were attributed to lymphoma, and 2 of those occurred following systemic transformation.
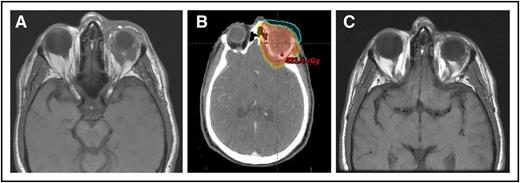
(A) A 64-year-old man with MZL of the left orbit. (B) An intensity-modulated RT plan of 24 Gy was designed, but only 4 Gy was delivered with near-CR obtained. (C) Seven months’ follow-up after only 4 Gy with no progression.
(A) A 64-year-old man with MZL of the left orbit. (B) An intensity-modulated RT plan of 24 Gy was designed, but only 4 Gy was delivered with near-CR obtained. (C) Seven months’ follow-up after only 4 Gy with no progression.
Although orbital MZL is almost always confined to the orbit at presentation, its natural history, as with other MZLs, is to occasionally emerge in other sites.2 With long, meticulous follow-up, relapse-free survival numbers worsen over time, but the distant relapse events are rarely lethal. Median overall survival in this series was longer than 250 months. About one-third of MALT lymphomas are disseminated up front,3 and, with improving imaging, we currently upstage even more patients at diagnosis and detect recurrences earlier.
Involvement of the ocular adnexa requires special attention regardless of stage. Recommending a quick, effective, and long-lasting local control, uniquely available with radiation alone, is important because of the risk to vision with even minimal progression of the disease. All patients in this report were indeed symptomatic.
As demonstrated in this series, a 3-decade policy of using RT for full eradication of the tumor and thus obtaining an irreversible local control (even in advanced stages) was highly successful. When RT was avoided in 15 patients, nearly one-half had orbital relapse or progression.
Advances in tumor imaging and radiation treatment planning, targeting, and delivery as well as a larger menu of RT systems (including intensity-modulated RT, electrons, and protons) provide an opportunity for more conformal treatment and a possibility of safely reducing the irradiated volume in the orbit in selected cases, particularly when the MZL is limited to the conjunctiva or lacrimal gland. Yet, the standard recommendation for most cases is to still include the full orbital contents unless the disease is confined to the conjunctiva (see figure).
The investigators from the University of Miami highlight the issue of radiation dose. They claim that their data show a correlation between inferior progression-free survival (mostly related to nonorbital events) and lower orbital radiation dose. This assertion, if accepted, could potentially influence the RT dose prescribed to the orbit and, in fact, to the eye, with its sensitive components. The dose they imply is higher than what international and national dose guidelines recommend; thus, the quality of the observed dose-outcome data requires further scrutiny.
It appears that in the more than 3 decades of patient inclusion in the study, there has not been a consistent RT dose policy. It is unclear how dose decisions were made, yet, in general, the dose hovered around 30 Gy. The more recent patients (since 2003) have received 30.6 Gy in 1.8 Gy per fraction doses, whereas earlier there was more RT dose variance. The investigators selected 2 dose groups: <30.6 Gy and ≥30.6 Gy. Notably, there was no accounting for the important biologic effect of fraction size. Radiobiologically, programs with larger doses per fraction are more effective; thus, a smaller total dose is required to achieve the same tumor cell-kill effect. This is normally an important factor in comparing the effect of different radiation programs. Notably, the mean doses of the “low-dose” group and of the “higher dose” group were 29 Gy and 33 Gy, respectively. When not accounting for fraction size or performing quality dose distribution in the target, these differences are biologically and clinically negligible. Indeed, the local effect was very similar: of the 20 low-dose patients, 18 achieved CR, 2 achieved partial remission (PR; unclear if ever progressed), and 4 had relapses; of the 78 patients in the ≥30.6 Gy group, only 1 had a PR and 1 relapsed. The observed Kaplan-Meier difference (P = .0058) is based on only 5 events and could be easily influenced by poor dose distribution related to inferior old radiation techniques or other factors that are not detailed. The observation that orbital RT dose also affected relapse remote from the orbit supports the concern that the dose/treatment period was merely a surrogate of other factors related to quality of staging or diagnosis at that period.
In recent years, the lymphoma radiation oncology community endorsed the use of lower doses to treat early-stage indolent lymphomas. This policy applies not only to follicular lymphomas, but also to MZLs. The recommendations are based not only on clinical experience and retrospective data, but also are supported by a large prospective randomized study comparing showing equivalent disease control with 24 Gy (in 2-Gy fractions) compared with the old standard of 40 to 45 Gy.4
The dose recommended for MZLs (nodal or extranodal) by the National Comprehensive Cancer Network is 24 to 30 Gy.5 The International Lymphoma Radiation Oncology Group recommendations specifically for orbital MZL are in the range of 24 to 25 Gy, with a preference to smaller fractions of 1.5 to 1.8 Gy.6 This experience is supported by several studies documenting excellent control with this dose range.7 Some suggest that conjunctival lesions are controlled with the lower dose range, whereas for deeper lesions 30 Gy will suffice. Only rare cases of bulky tumors or those that are slow to respond may require a dose of 36 Gy.
More recently, a very low dose of only 4 Gy (2 Gy ×2) was shown to be adequately effective in a prospective randomized study from the United Kingdom, and a group from Stanford reported on their favorable experience with this low-dose schedule.8,9
Although orbital radiation is usually well-tolerated, long-term complications, such as premature cataract and dryness, are dose-dependent—and exceeding 36 Gy may increase risks of ischemic retinopathy, optic atrophy, corneal ulceration, and neovascular glaucoma. RT of orbital MZL rarely needs to exceed 30 Gy, and I hope that the readers of the University of Miami study will not conclude that the higher the orbital RT dose, the better.
Conflict-of-interest disclosure: The author declares no competing financial interests.