In this issue of Blood, complimentary studies by J. Li et al1 and H. Li et al2 identify the transcription factor ZEB2 as a critical regulator of multilineage differentiation in both normal and malignant hematopoiesis. In particular, these studies show that ZEB2 is an inhibitor of normal granulocyte production, and in acute myeloid leukemia (AML), antagonizing ZEB2 function releases the granulocytic differentiation block, creating an antileukemic therapeutic effect.
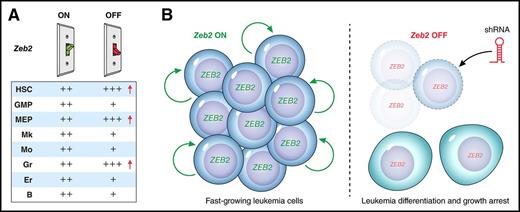
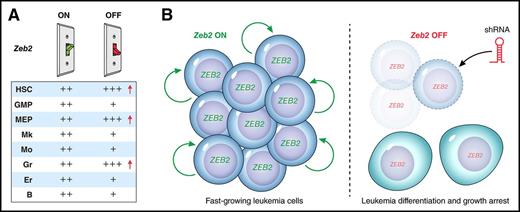
ZEB2 is a differentiation switch in normal hematopoiesis and leukemogenesis. (A) Cartoon illustration of Zeb2 “ON” and “OFF” expression switches (depicted as green and red, respectively), indicating that with Zeb2 expression, all hematopoietic stem, progenitor, and mature lineages are produced at normal numbers (++). However, on deletion of Zeb2 expression, multilineage differentiation and progenitor production are perturbed. Red arrows highlight increased HSC, MEP, and granulocytes in the absence of Zeb2. (B, left) Illustration of ZEB2 expressing AML cells undergoing proliferation and self-renewal. (B, right) ZEB2 shRNA-mediated knockdown results in differentiation and decreased proliferation of AML cells. B, B-cell; Er, erythrocyte; GMP, granulocyte-monocyte progenitor; Gr, granulocyte; MEP, megakaryocyte-erythrocyte progenitor; Mk, mature megakaryocyte; Mo, monocyte.
ZEB2 is a differentiation switch in normal hematopoiesis and leukemogenesis. (A) Cartoon illustration of Zeb2 “ON” and “OFF” expression switches (depicted as green and red, respectively), indicating that with Zeb2 expression, all hematopoietic stem, progenitor, and mature lineages are produced at normal numbers (++). However, on deletion of Zeb2 expression, multilineage differentiation and progenitor production are perturbed. Red arrows highlight increased HSC, MEP, and granulocytes in the absence of Zeb2. (B, left) Illustration of ZEB2 expressing AML cells undergoing proliferation and self-renewal. (B, right) ZEB2 shRNA-mediated knockdown results in differentiation and decreased proliferation of AML cells. B, B-cell; Er, erythrocyte; GMP, granulocyte-monocyte progenitor; Gr, granulocyte; MEP, megakaryocyte-erythrocyte progenitor; Mk, mature megakaryocyte; Mo, monocyte.
ZEB2 is most widely known as an inducer of epithelial-to-mesenchymal transition (EMT), the process of converting from a mature epithelial-like state to an immature mesenchymal state with increased migratory and invasive behavior. EMT occurs normally in tissue morphogenesis, including during embryonic organ development and wound healing. Several transcription factors including Snail/Slug, Twist, and Zeb1/2 contribute to EMT, and these pathways remain intact in many cancer cells. ZEB2 expression can directly induce EMT in a variety of solid tumor types, and can thereby promote metastasis.3,4 Consistent with the EMT function of ZEB2, new findings by J. Li et al and H. Li et al uncover a crucial theme to ZEB2 biology in regulating the balance between stemness and differentiation in normal hematopoiesis and leukemia.1,2
Previously, it was shown that Zeb2 expression is essential for embryonic hematopoietic stem and progenitor cell (HSPC) differentiation in the fetal liver.5 With the use of a mouse model harboring conditional deletion of Zeb2 in adult hematopoietic cells, J. Li et al1 report that Zeb2 controls hematopoietic stem cell (HSC) numbers, as well as differentiation of myeloid progenitors, B-cell and myeloid precursors, and terminally differentiated cells. Strikingly, Zeb2 knockout results in loss and/or aberrant morphology of many mature cell types, including monocytes, B-cells, erythrocytes, and platelets, but causes a significant increase in the number of granulocytes1 (see figure, panel A). Moreover, conditional Zeb2 knockout mice develop splenomegaly accompanied by HSPC infiltration, with a corresponding increase in extramedullary hematopoiesis. Evidence from J. Li et al1 suggests that, at least in part, Zeb2 functions to integrate signals from different cytokines to mediate its effects on differentiation.
The fundamental changes to HSPCs, giving rise to hematologic malignancies, include attenuated hematopoietic differentiation and gain of self-renewal. The resulting abnormal blasts accumulate and move from the bone marrow into the peripheral blood and colonize additional sites such as the spleen and liver, a process reminiscent of EMT in metastatic disease. Using high-throughput shRNA screens comparing AML and non-AML cancer cell lines in vitro, and validation in a murine model of AML in vivo, H. Li et al2 identified ZEB2 as an AML-specific dependency. Interestingly, knockdown of ZEB2 in AML cells promoted the expression of genes associated with granulocytic differentiation, and in addition to displaying some morphological features of differentiation, arrested leukemia cell growth (see figure, panel B). Finally, H. Li et al2 show that the miR-200 negative-feedback loop present in solid cancers that potentiates ZEB2-mediated EMT6,7 is also intact in AML cells.
These studies by J. Li et al and H. Li et al corroborate and complement one another in several ways.1,2 First, each reports that ZEB2 is highly expressed in HSPCs and in AML. Second, a granulocyte differentiation threshold or blockade is released when ZEB2 is repressed or deleted in normal and malignant hematopoietic cells. Thus, cancer cells co-opt ZEB2 to inhibit differentiation and promote stemness. In agreement with these findings, another recent study identified invasion, migration, and metastasis genes, including Zeb2, associated with aggressive, early-onset, HSC-derived AML, which were not present in slower-growing, more differentiated, progenitor-derived AML.8 Altogether, these studies remind us of the complexity of balancing stemness and differentiation with many other processes such as migration, invasion, and proliferation in hematopoiesis and leukemia. But is ZEB2 a master “on/off” switch that integrates all these processes? Moving forward, additional work needs to be done to more precisely elucidate the molecular mechanisms at play and to investigate the potential development and use of ZEB2 pathway inhibitors as an antileukemic therapy. Such a therapy will likely have a wide range of applicability not only for AML but also in early T-cell precursor acute lymphoblastic leukemia9 and solid cancers such as breast,10 colorectal,11 and liver cancers.12 However, careful consideration will need to be given to limit the toxicity of this type of differentiation therapy on the remaining normal immune cell populations, which also rely on ZEB2. In sum, these findings solidify a role for ZEB2 as an essential regulator of normal and malignant hematopoietic differentiation and suggest a closer look at EMT pathways as therapeutic candidates in leukemia and in other malignant contexts is warranted.
Conflict-of-interest disclosure: The author declares no competing financial interests.