Key Points
Angiocrine Bmp2 signaling in the liver controls tissue and serum iron concentrations via regulation of hepcidin expression in hepatocytes.
Liver-specific angiocrine signaling is essential for the metabolic homeostasis of the whole organism.
Abstract
Microvascular endothelial cells (ECs) display a high degree of phenotypic and functional heterogeneity among different organs. Organ-specific ECs control their tissue microenvironment by angiocrine factors in health and disease. Liver sinusoidal endothelial cells (LSECs) are uniquely differentiated to fulfill important organ-specific functions in development, under homeostatic conditions, and in regeneration and liver pathology. Recently, Bmp2 has been identified by us as an organ-specific angiokine derived from LSECs. To study angiocrine Bmp2 signaling in the liver, we conditionally deleted Bmp2 in LSECs using EC subtype-specific Stab2-Cre mice. Genetic inactivation of hepatic angiocrine Bmp2 signaling in Stab2-Cre;Bmp2fl/fl (Bmp2LSECKO) mice caused massive iron overload in the liver and increased serum iron levels and iron deposition in several organs similar to classic hereditary hemochromatosis. Iron overload was mediated by decreased hepatic expression of hepcidin, a key regulator of iron homeostasis. Thus, angiocrine Bmp2 signaling within the hepatic vascular niche represents a constitutive pathway indispensable for iron homeostasis in vivo that is nonredundant with Bmp6. Notably, we demonstrate that organ-specific angiocrine signaling is essential not only for the homeostasis of the respective organ but also for the homeostasis of the whole organism.
Introduction
Endothelial cell (EC)–derived paracrine factors acting in organ-specific vascular niches are defined collectively as angiocrine factors/angiokines.1 Angiokines are involved, for example, in organ-specific tissue homeostasis and regeneration in bone marrow, lung, and liver. Recently, the Bmp family member Bmp2 was identified by us2 and others3 as an angiokine that is preferentially expressed by liver sinusoidal endothelial cells (LSECs), but not by ECs of most other organs or of lymphatic vessels. Proangiogenic and proinflammatory effects of Bmp2 have been studied in detail in cultured ECs.4-6 Few studies, however, have addressed potential angiocrine functions of Bmp2 in vivo.7-9
Recently, 2 nonredundant signaling pathways have been proposed that control hepatic hepcidin expression and iron homeostasis.10 One pathway comprises Bmp6 signaling via type I (Bmpr1a/Alk3) and type II (Bmpr2) receptors and Smad phosyphorylation in hepatocytes.11-14 The other pathway comprises hepcidin induction via activation of a Hfe/Tfr2/Hjv/Bmp type II receptor complex. The authors proposed that the second pathway is activated independently from Bmp6 by another, so far unknown, Bmp ligand they hypothesized to be Bmp2.10 Supporting this notion, genetic evidence suggests a role of Bmp2 in classic hereditary hemochromatosis as a phenotypic modifier.15,16 In addition, Bmp2 has been shown to be upregulated under pathological conditions such as thalassemia in mice and multiple myeloma in humans and to modulate hepcidin expression in hepatocytes and/or nonparenchymal liver cells.17,18 Here, we show that LSEC-derived Bmp2 represents a key angiokine maintaining normal iron metabolism under homeostatic conditions in vivo.
Study design
Animals
Bmp2 loss of function in LSECs (Stab2-Cretg/wt;Bmp2fl/fl=Bmp2LSECKO) was achieved by crossing Stab2-Cretg/wt;Bmp2fl/wt with Bmp2fl/fl19 mice. Animal experiments were approved by the animal ethics committee (Regierungspraesidium Karlsruhe).
Iron and hepcidin quantification
Serum iron levels were measured with a Dimension Vista 1500 analyzer (Siemens). Mouse tissue lysates and serum samples were measured with an Iron Assay Kit (Sigma-Aldrich) and Hepcidin-Murine Compete Enzyme-Linked Immunosorbent Assay (Intrinsic LifeSciences).
Immunohistochemistry, in situ hybridization, and immunofluorescence
Acetone-fixed cryosections (8 µm) were stained as described20 and photographed using an ECLIPSE Ni-E microscope (Nikon). In situ hybridization was carried out using the RNAscope 2.5 HD Brown kit (Advanced Cell Diagnostics).
Antibodies
Primary antibodies included the following: mouse anti–Stabilin-2 #3.1, mouse anti–Stabilin-1 #1.26,20 rabbit anti-Lyve1 (ReliaTech), rabbit anti–glutamine synthetase (GS; Santa Cruz), and goat anti–arginase-I (Santa Cruz). Appropriate secondary antibodies were used (Dianova).
Quantitative reverse-transcription polymerase chain reaction (qRT-PCR)
Liver RNA samples and complementary DNA were generated as described.2 Primers were designed using NCBI Primer-BLAST. qRT-PCR was performed in an Mx3005P qPCR system (Stratagene) using SYBR Green PCR Master-Mix (Applied Biosystems).
Primary murine cells
Microarray data
Gene expression profiling was performed using MoGene-1_0-st-v1-type arrays (Affymetrix). The raw fluorescence intensity values were normalized, and differential gene expression was analyzed with 1-way analysis of variance (SAS Institute). The transcriptomic data are deposited in the Gene Expression Omnibus database (http://www.ncbi.nlm.nih.gov/geo/; accession number GSE90506).
Results and discussion
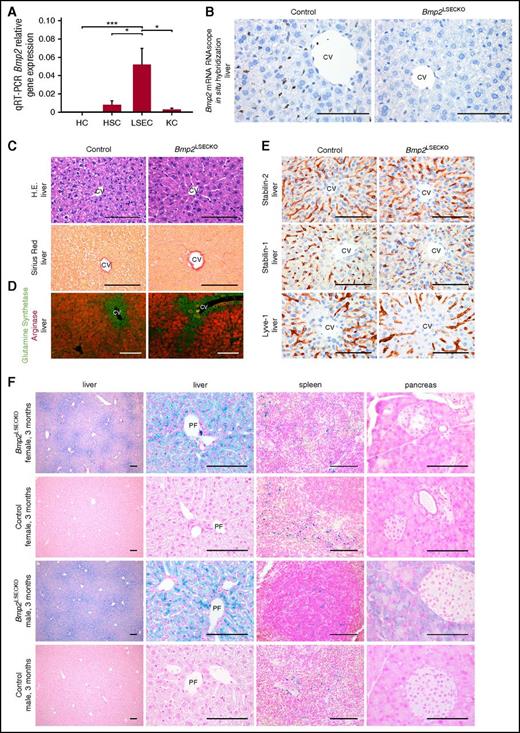
LSECs expressed much higher levels of Bmp2 messenger RNA (mRNA) than hepatocytes, Kupffer cells, and stellate cells, indicating that LSECs are the major source of Bmp2 expression in the liver (Figure 1A); in addition, Bmp2 was expressed by LSECs, but not other liver ECs, such as central vein ECs (Figure 1B). To study angiocrine Bmp2 signaling in the liver, we conditionally deleted Bmp2 in LSECs using EC subtype-specific Stab2-Cre mice. Reporter activity of Stab2-Cre;R26YFP mice was restricted to the hepatic endothelium–sparing hepatocytes and other nonparenchymal liver cells (supplemental Figure 1A-B, available on the Blood Web site). Stab2-Cre;Bmp2fl/fl (Bmp2LSECKO) mice survived into late adulthood without any gross abnormalities (supplemental Figure 2A-C). Bmp2 expression and protein levels were decreased in the liver of Bmp2LSECKO mice, whereas Bmp2 protein levels in the spleen and in the serum of Bmp2LSECKO and control mice varied between sexes (Figure 1B; supplemental Figure 2D-E). These findings confirmed that angiocrine Bmp2 signaling in the liver was successfully abolished in Bmp2LSECKO mice.
Angiocrine Bmp2 signaling in the liver controls tissue iron content and distribution. (A) Comparative qRT-PCR analysis of Bmp2 mRNA expression in LSECs, hepatocytes (HC), Kupffer cells (KC), and stellate cells (HSC) isolated from livers of wild-type (WT) adult C57Bl/6 mice (n = 5). β-2-Microglobulin was used as housekeeping gene. *P < .05; ***P < .001. (B) Bmp2 mRNA in situ hybridization of liver sections of Bmp2LSECKO mice in comparison with WT controls (n = 3). Scale bar, 100 μm (×60). CV, central vein. (C) Hematoxylin and eosin (H.E.) and Sirius red staining of liver sections of Bmp2LSECKO mice in comparison with WT controls (n = 6). Scale bar, 100 μm (×60). (D) Coimmunofluorescence of GS and arginase in liver (n = 5). Scale bar, 100 μm (×20). (E) Immunohistochemistry of LSEC markers in livers of Bmp2LSECKO and control mice (n = 5). Scale bar, 100 μm (×60). (F) Prussian blue staining demonstrating iron deposition in liver, spleen, and pancreas of Bmp2LSECKO (female, n = 5; male, n = 5). Scale bar, 100 μm (first column, ×10; third column, ×40; second and fourth columns, ×60). PF, portal field.
Angiocrine Bmp2 signaling in the liver controls tissue iron content and distribution. (A) Comparative qRT-PCR analysis of Bmp2 mRNA expression in LSECs, hepatocytes (HC), Kupffer cells (KC), and stellate cells (HSC) isolated from livers of wild-type (WT) adult C57Bl/6 mice (n = 5). β-2-Microglobulin was used as housekeeping gene. *P < .05; ***P < .001. (B) Bmp2 mRNA in situ hybridization of liver sections of Bmp2LSECKO mice in comparison with WT controls (n = 3). Scale bar, 100 μm (×60). CV, central vein. (C) Hematoxylin and eosin (H.E.) and Sirius red staining of liver sections of Bmp2LSECKO mice in comparison with WT controls (n = 6). Scale bar, 100 μm (×60). (D) Coimmunofluorescence of GS and arginase in liver (n = 5). Scale bar, 100 μm (×20). (E) Immunohistochemistry of LSEC markers in livers of Bmp2LSECKO and control mice (n = 5). Scale bar, 100 μm (×60). (F) Prussian blue staining demonstrating iron deposition in liver, spleen, and pancreas of Bmp2LSECKO (female, n = 5; male, n = 5). Scale bar, 100 μm (first column, ×10; third column, ×40; second and fourth columns, ×60). PF, portal field.
Routine hematoxylin and eosin staining of various organs of Bmp2LSECKO mice including the liver did not reveal obvious abnormalities (Figure 1C; supplemental Figure 3A). Upon Sirius red staining, no hepatic fibrosis was detected (Figure 1C). Liver zonation as determined by expression of GS or arginase was not affected in Bmp2LSECKO mice (Figure 1D). Expression of marker proteins for LSECs such as Stab1, Stab2, and Lyve-1 and for continuous ECs such as CD31 was also not altered in Bmp2LSECKO livers (Figure 1E; supplemental Figure 3B). On the contrary, Prussian blue staining revealed massive iron overload in the liver (Figure 1F). Iron deposits within hepatocytes displayed a zonal pattern with a preferential periportal distribution (Figure 1F). Confirming LSEC-specific expression and function of Bmp2, Alb-Cre;Bmp2fl/fl mice did not show alterations in iron content (supplemental Figure 3C). Although iron deposits in the spleen did not show any differences between Bmp2LSECKO mice and controls (Figure 1F), iron deposition was increased in the pancreas (Figure 1F) and the heart of male, but not female Bmp2LSECKO mice (supplemental Figure 4).
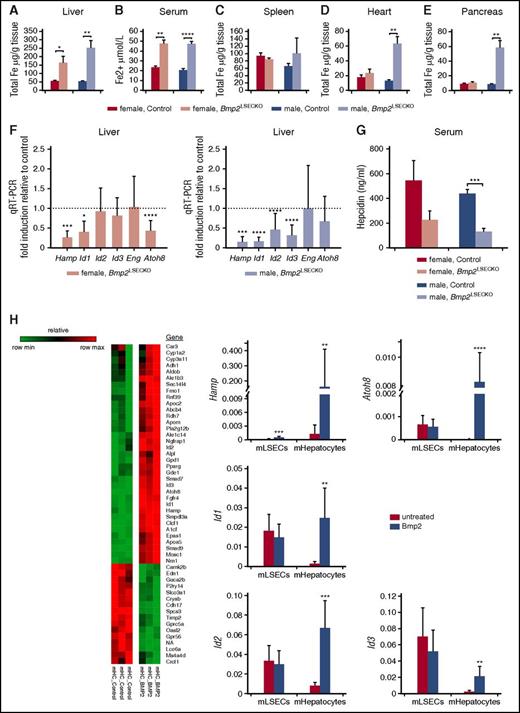
Iron content was significantly increased in Bmp2LSECKO liver tissue of male and female mice, in the heart and pancreas of male Bmp2LSECKO mice, as well as in serum of both sexes, whereas it was not altered in the spleen (Figure 2A-E). Molecules involved in either Bmp2 signaling or iron metabolism such as Ferroportin (Scl40a1), erythroferrone (Fam132b), the Bmp type I/II receptors such as Acvr1/Alk2, Bmpr1a/Alk3, and Bmpr2 were also not altered except for Bmp6 (supplemental Figure 5A-C). Hemoglobin levels did not show significant differences (supplemental Figure 6A). Furthermore, blood cell counts, liver function tests, electrolytes, total protein, and urea as well as glucose were normal in Bmp2LSECKO mice (supplemental Figure 6B-C). Nevertheless, hepcidin expression in the liver, but not the spleen, and hepcidin serum levels were downregulated in Bmp2LSECKO mice (Figure 2F-G; supplemental Figure 5D).
Angiocrine Bmp2 signaling in the liver controls tissue and serum iron concentrations via regulation of hepatocyte hepcidin expression. (A-E) Iron concentration in (A) liver, (B) serum, (C) spleen, (D) heart, and (E) pancreas of Bmp2LSECKO and control mice (female, n = 5; male, n = 5). *P < .05; **P < .01; ****P < .0001. (F) qRT-PCR of Hamp, Id1, Id2, Id3, Endoglin (Eng), and Atoh8 in liver of Bmp2LSECKO and control mice (female, n = 5; male, n = 5). β-Actin was used as housekeeping gene. *P < .05; ***P < .001; ****P < .0001. (G) Serum hepcidin levels of Bmp2LSECKO and control mice as measured by enzyme-linked immunosorbent assay (female, n = 5; male, n = 5). ***P < .001. (H) Gene expression heat map of murine hepatocytes stimulated with Bmp2 for 24 hours (left panel). Bmp2-dependent expression of Hamp, Id1, Id2, Id3, and Atoh8 was quantified by qRT-PCR (right panel) of hepatocytes stimulated with Bmp2 for 24 hours and of murine LSECs (mLSECs) stimulated with Bmp2 for 48 hours. β-Actin was used as housekeeping gene. *P < .05; **P < .01; ***P < .001; ****P < .0001.
Angiocrine Bmp2 signaling in the liver controls tissue and serum iron concentrations via regulation of hepatocyte hepcidin expression. (A-E) Iron concentration in (A) liver, (B) serum, (C) spleen, (D) heart, and (E) pancreas of Bmp2LSECKO and control mice (female, n = 5; male, n = 5). *P < .05; **P < .01; ****P < .0001. (F) qRT-PCR of Hamp, Id1, Id2, Id3, Endoglin (Eng), and Atoh8 in liver of Bmp2LSECKO and control mice (female, n = 5; male, n = 5). β-Actin was used as housekeeping gene. *P < .05; ***P < .001; ****P < .0001. (G) Serum hepcidin levels of Bmp2LSECKO and control mice as measured by enzyme-linked immunosorbent assay (female, n = 5; male, n = 5). ***P < .001. (H) Gene expression heat map of murine hepatocytes stimulated with Bmp2 for 24 hours (left panel). Bmp2-dependent expression of Hamp, Id1, Id2, Id3, and Atoh8 was quantified by qRT-PCR (right panel) of hepatocytes stimulated with Bmp2 for 24 hours and of murine LSECs (mLSECs) stimulated with Bmp2 for 48 hours. β-Actin was used as housekeeping gene. *P < .05; **P < .01; ***P < .001; ****P < .0001.
To further analyze angiocrine Bmp2 signaling in vitro, we analyzed primary mouse hepatocytes exposed to exogenous Bmp2. Bmp2 stimulation resulted in the induction of 35 genes with a fold change > 2 and repression of 16 genes with a fold change < −2 (Figure 2H). Among these were well-established Bmp response genes such as Id1, Id2, Id3, Atoh8, and Hamp1/Hepcidin. In contrast, primary mLSECs did not show similar changes in expression of these genes (Figure 2H).
Therefore, angiocrine Bmp2 signaling directly affected iron homeostasis via regulation of hepatocytic Hamp1/hepcidin expression. Conspicuous periportal zonation of iron overload in the liver in Bmp2LSECKO mice was similar to Acvr1(Alk2)–deficient mice in contrast to centrilobular zonation in Bmp6-, Bmpr1a-, and Bmpr2-deficient mice.11-14 Lack of iron deficiency in the spleen was also similar to Acvr1(Alk2)-deficient mice, whereas iron overload in the heart and pancreas rather resembled Bmp6-deficient mice. Altogether, this indicates that Bmp2 and Acvr1 rather signal within the same pathway that complements the one controlled by Bmp6 and Bmpr1a/Alk3. Most notably, angiocrine Bmp2 signaling in the liver does not only act locally, but regulates iron homeostasis also at distant sites such as the pancreas and heart by activating hepatocyte expression of the hepatic hormone hepcidin. Thus, we demonstrate that organ-specific angiocrine EC functions are indispensable not only for the homeostasis of their organ of origin but also for the homeostasis of the whole organism.
The data reported in this article have been deposited in the Gene Expression Omnibus database (accession number GSE90506).
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Monica Adrian, Jochen Weber, Hiltrud Schönhaber, Maria Muciek, Brigitte Landrock, Elisabeth Seelinger, and Alexandra Müller for excellent technical support and Hellmut Augustin for advice and discussions during the preparation of the manuscript and acknowledge the support of the Core Facility Live Cell Imaging Mannheim at the Centre for Biomedicine and Medical Technology Mannheim (German Research Foundation grant DFG INST 91027/9-1 FUGG).
This work was supported in part by grants from the German Research Foundation (Deutsche Forschungsgemeinschaft) GRK2099/RTG2099, project 7 (C.G. and S.G.), SFB-TR23, project B1 (C.G. and S.G.), and SFB-TR77, project C3 (S.G.), and by a scholarship from the Germany Society of Dermatology (Deutsche Dermatologische Gesellschaft), the Arbeitsgemeinschaft Dermatologische Forschung (C.G.).
Authorship
Contribution: P.-S.K., V.O., K.S., S.G., and C.G. designed the study concept and design; P.-S.K., V.O., F.U., C.S., T.L., A.D., T.H., M.M., J.Z., S.S., K.B.-H., H.G., B.S.-D., K.K., B.A., K.S., S.G., and C.G. conducted the experimental work and the analysis and interpreted the data; S.G. and C.G. wrote the original draft; all the authors revised and approved the manuscript before submission.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Philipp-Sebastian Koch, Klinik für Dermatologie, Venerologie, und Allergologie, Universitätsmedizin Mannheim, D-68135 Mannheim, Germany; e-mail: philipp.koch@umm.de; and Cyrill Géraud, Klinik für Dermatologie, Venerologie, und Allergologie, Universitätsmedizin Mannheim, D-68135 Mannheim, Germany; e-mail: cyrill.geraud@umm.de.
References
Author notes
P.-S.K. and V.O. contributed equally to this study.
S.G. and C.G. contributed equally to this study.