In this issue of Blood, Bouska et al give an excellent example of an integrated molecular approach applied to high-grade B-cell lymphoma with the molecular Burkitt lymphoma (BL) signature.1 This study has several practical implications regarding (1) the concept of the pathological entity, (2) the understanding of the different mechanisms at work in patients who apparently have the same disease, and (3) the impact that a comprehensive molecular approach can have on the identification of novel therapeutic targets.
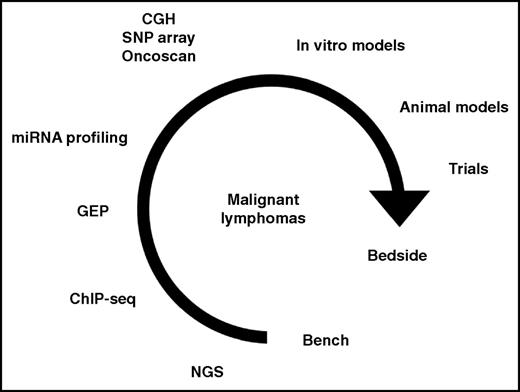
The integration of various techniques as the basis for translational research in malignant lymphomas. CGH, comparative genomic hybridization; ChIP-seq, chromatin immunoprecipitation sequencing; GEP, gene expression profiling; miRNA, microRNA; NGS, next-generation sequencing (including whole-genome sequencing, whole-exome sequencing, targeted sequencing, and RNA sequencing); SNP, single-nucleotide polymorphism.
The integration of various techniques as the basis for translational research in malignant lymphomas. CGH, comparative genomic hybridization; ChIP-seq, chromatin immunoprecipitation sequencing; GEP, gene expression profiling; miRNA, microRNA; NGS, next-generation sequencing (including whole-genome sequencing, whole-exome sequencing, targeted sequencing, and RNA sequencing); SNP, single-nucleotide polymorphism.
For decades, the classification of malignant lymphomas was based on cell morphology, beginning with the Revised European-American Classification of Lymphoid Neoplasms and then the third, fourth, and revised editions of the World Health Organization (WHO) Classification of Tumors of Hematopoietic and Lymphoid Tissues, which established that a pathological entity is defined by the amalgamation of clinical, morphological, phenotypic, cytogenetic, and molecular characteristics, as well as the identification of its normal counterpart, if possible.2-7 However, the development of more and more sensitive molecular techniques, which moved from limited gene expression profiling and the discovery of the alterations affecting single genes at the beginning of this century to whole-exome or genome sequencing, copy-number alteration (CNA) analysis, or liquid biopsy from circulating free DNA, has dramatically improved our knowledge of the pathobiology of these neoplasms. In acute myeloid leukemia, the French-American-British classification has been completely overcome by a molecular approach, which distinguishes different entities based on founder lesions and has important therapeutic implications.6-8 The same process is ongoing in malignant lymphomas, although a molecular subclassification is not yet systematically used for diagnosis, therapeutic decisions, and drug discovery. In the revised WHO classification, some hints of the molecular subclassification of malignant lymphomas are starting to emerge (eg, the classification of diffuse large B-cell lymphomas [DLBCL] into germinal center B-cell and activated B-cell types).5,7,9 The article by Bouska et al underlines that lymphoid tumors sharing the same gene signature can be further classified based on their molecular characteristics.1 This is, for instance, the case of adult and pediatric neoplasms with a molecular BL signature, which have completely different behavior. Conversely to pediatric molecular BL, adult molecular BL reveals either unique or more frequent genomic aberrations (del13q14, del 17p, gain 8q24, and gain 18q21) and is associated with effectors of chronic B-cell receptor (BCR)→NF-κB signaling.1 These findings refer to Western cases, which are the only ones studied by the authors.1 Endemic tumors carry a partly different mutational landscape and show an inverse correlation between Epstein-Barr virus infection and the number of mutations.10 Thus, it may be expected that the same comprehensive approach applied to endemic cases would reveal further heterogeneity. Notably, 2 of the adult cases reported by Bouska et al were characterized by the lack of MYC rearrangement and the occurrence of 11q aberrations.1 This suggests their possible inclusion in the new provisional category of the revised WHO classification, Burkitt-like lymphoma with 11q aberration.5,7 Finally, yet importantly, 8 of 24 adult cases with a molecular BL signature carried double hits (ie, BCL2 and MYC translocations). These cases would now be included in the new category of high-grade B-cell lymphoma with double or triple hit in the revised WHO classification.5,7 Seven of them showed the same mutational landscape as BL except for a KMT2D mutation frequency like follicular lymphoma. Thus, the same gene signature includes cases that can be further subclassified based on the fine-tuning of their molecular characteristics.
On pathogenetic grounds, integrative analysis identified an interrelated gene network affected by CNAs and mutations, leading to disruption of the p53 pathway and BCR→phosphatidylinositol 3-kinase or NF-κB activation.1 Recurrent CNAs/mutations were identified in genes associated with p53 signaling, cell-cycle regulation, or apoptosis. Loss of p53 function by copy-number loss or mutation occurred in half of adult molecular BL. Interestingly, cases carrying TP53 copy loss and copy neutral loss of heterozygosity also had TP53 mutation, but not vice versa, indicating that mutation may occur earlier than CNA.1 It would be of interest to systematically explore this finding in other lymphoid tumors carrying either type of TP53 alteration. Another important observation was the occurrence of gain/amplification of MIR17HG/miR17∼92 and its paralog loci in 50% of adult molecular BL, a prevalence two times higher than that of pediatric cases. Interestingly, adult molecular BL patients with MIR17HG gains had worse overall survival and enrichment of gene signatures associated with immune suppression or hypoxia and chemoresistance. Despite MIR17HG gains having a negative correlation with MYC expression in tumors, the fact that the expression of miR17∼92 was higher in molecular BL than in DLBCL and germinal center B cells suggests a distinct role for miR17∼92 in BL pathogenesis.1 Thus, a series of elegant in vitro experiments carried out by the authors on 6 BL cells lines revealed that miR17∼92 expression induced BCR signaling activation.1 The loss of functional miR17∼92 led to diminished BCR signaling in BL cell lines, thus confirming a positive role in B-cell activation.1
Based on the latter finding and the knowledge that targets of miR17∼92 include FCGR2B, modulating BTK function via SHIP and PLCγ, the authors postulated sensitivity to BTK inhibitors.1 This assumption was supported by growth inhibition by ibrutinib in the 6 BL cell lines tested in a time- and dose-dependent manner.1 Accordingly, patients with molecular BL and MIR17HG amplification (which is characterized by an unfavorable prognosis) might benefit from the use of BTK inhibitors.
The study by Bouska et al represents an excellent example of the way in which an integrated molecular approach can contribute to the better subclassification of malignant lymphomas belonging to the same category, as well as to a better understanding of their pathogenesis and novel targeted therapy discovery.1 It is clear that only the blend of information produced by the application of different technologies to the study of a given hematolymphoid tumor (as exemplified in the figure) can actually promote translational research and precision medicine with benefit for the patient.
Conflict-of-interest disclosure: The author declares no competing financial interests.