Abstract
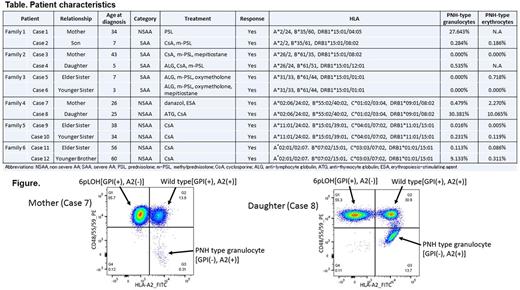
[Background] Aplastic anemia (AA) is a syndrome characterized by pancytopenia and bone marrow hypoplasia caused by various factors. When AA occurs in family members, congenital AA is usually suspected. However, some anecdotal reports have described the occurrence of AA in family members who did not show any signs or laboratory findings compatible with congenital AA and instead represented an acquired feature, such as a good response to immunosuppressive therapy. Studying such familial AA without evident congenital features may help to clarify the genetic or environmental factors that are closely associated with susceptibility to AA. [Objectives/Methods] To characterize non-congenital AA that occurred in family members, we reviewed the clinical records of about 3000 AA patients who were referred to our clinic for the examination of glycosylphosphatidylinositol-anchored protein-deficient (PNH-type) blood cells from 1999 to 2017 and found 6 pairs of AA patients in 6 different families (Table). Three pairs were parents and children, and the other three pairs were siblings. None of the families had malformations or family histories except for the affected pairs. All patients' samples were subjected to high-sensitivity flow cytometry for detecting PNH-type cells and HLA genotyping. Two pairs of patients (Cases 7 and 8, and Cases 9 and 10) who were diagnosed after 2015 were also examined for the presence of HLA class I-lacking leukocytes using monoclonal antibodies specific to class I HLA alleles, and for the presence of myeloid malignancy-related gene abnormalities using a next-generation sequencer. [Results] PNH-type granulocytes were detected in 9 of 12 cases at frequencies of 0.016% to 30.381%. Five pairs shared HLA-DRB1*15:01, which is known to be associated with PNH, while three pairs shared HLA-B*40:02, an HLA class I allele most frequently lost as a result of 6pLOH or allelic mutations. HLA-A allele-lacking leukocytes were detected in one of the two pairs studied (Figure). Unexpectedly, the lacked HLA alleles in the pair (Cases 7 and 8) were not B*40:02but A*02:06. No somatic mutations were found in 61 myeloid malignancy-related genes of the granulocytes from the 2 cases. All of 12 patients responded to immunosuppressive therapy (IST, 6 with cyclosporine alone and 4 with ALG/ATG+/-cyclosporine) and achieved transfusion independence. [Conclusions] The high prevalence of markers for immune pathophysiology, including PNH-type cells and HLA allele-lacking cells, the high frequency of DRB*15:01 and B*40:02, and a good response to IST in the 6 family pairs suggests that non-congenital familial AA is a typical type of immune-mediated bone marrow failure affected by the genetic background. The lack of the same HLA class I allele (A*02:06) in the mother (Case 7) and her daughter (Case 8) in their granulocytes suggests the involvement of a common environmental factor that induces the generation of cytotoxic T lymphocytes specific to common antigens presented by the HLA-A allele.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.