Background: Standard induction chemotherapy for acute myeloid leukemia (AML) with "7+3" regimen consisting of cytarabine and daunorubicin (DNR) yields a complete remission (CR) rate of 40-80%. Current practice, endorsed by the National Comprehensive Cancer Network, is to perform a repeat bone marrow assessment on day 14 (D14) of initial induction. A blast count greater than 5-10% with a marrow cellularity of 10-20% at that time suggests residual leukemia and recommendation is for a second round of induction chemotherapy. Most studies only note blast count as the key value in decision making. Large studies have confirmed a prognostic value of D14 bone marrow biopsy based on blast percentage, yet controversy lies in its use as treatment decision point. In this single center retrospective study, we evaluated the role of cellularity on clinical outcomes in patients with residual morphologic blasts on day-14 bone marrow biopsy.
Methods: All consecutive patients 18 years or older who received induction chemotherapy for newly diagnosed AML from 1/1/06 to 5/1/13 at the Lifespan Cancer Institute were identified. Outcomes were followed until 5/1/17. On D14 marrow assessment, patients were determined to have residual leukemia if the morphologic blast count was ≥5%, deemed to have an intermediate response (IR) if blasts counts were 5-19%, and considered hypocellular if the cellularity was <20%. Fisher's exact test and Wilcoxon rank-sum tests were performed to examine differences in categorical and continuous variables. CR was defined as a recovery bone marrow biopsy with <5% morphologic blasts in the setting of neutrophil and platelet recovery (Cheson et al, JCO 2003). Overall survival (OS) was defined as the time from diagnosis to the time of death or last follow up. OS curves were estimated using the Kaplan-Meier (KM) method and compared using the log-rank test. CR and OS were compared based on reinduction and cellularity using a logistic regression model. Negative and Positive predictive values (NPV, PPV) were calculated using standard 2x2 tables.
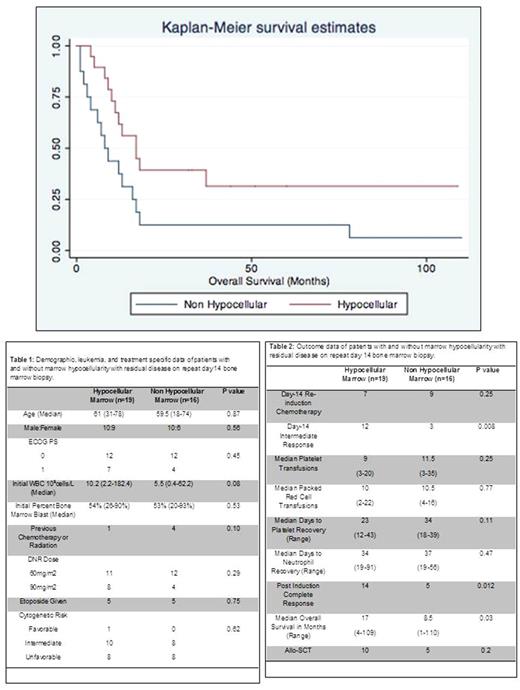
Results: Of 113 patients identified, 68 underwent D14 bone marrow biopsy and 35 had residual disease on D14 determined by blast count. Sixteen of these patients received reinduction. Nineteen had hypocellular bone marrows and 16 were non hypocellular. Between the hypocellular and non hypocellular groups no demographic or leukemia specific variables were significantly different (Table 1). In terms of outcome data, more patients with hypocellular D14 bone marrows attained an IR (12 of 19, 63%) compared to a non hypocellular marrow (3 of 16, 19%, p=.008). Furthermore, hypocellular D14 marrows showed improved post induction complete response (74% v. 31%, p=0.12) and improved median overall survival (17 v. 8.5 months, p=0.03, Figure 1) compared to non hypocellular D14 marrows. Based on logistic regression, there was no benefit for reinduction based on cellularity for either CR (OR 0.056, 95% CI 0.002-1.47) or OS (HR 1.96, 95% CI 0.4-9.6).
Using a blast count of ≥5% on the day-14 marrow assessment as a positive screening test for residual leukemia demonstrated PPV of 42%, NPV of 79%, sensitivity of 53% and specificity of 70% for achieving CR. Using the alternative cutoff of <20% blasts demonstrated PPV of 71%, NPV of 78%, sensitivity of 33%, and specificity of 95%. Using a non hypocellular marrow as a positive screening test, a PPV of 93% and NPV 67% was found with a sensitivity of 40% and a specificity of 97%.
Conclusions: In our single center retrospective review, we found that D14 bone marrow hypocellularity significantly predicted CR and OS in patients with residual morphologic blasts. We found no benefit to additional chemotherapy based on D14 marrow assessment in terms of attaining CR or improvement in OS. Furthermore, there was no benefit for reinduction based on D14 marrow cellularity using logistic regression. There is improved specificity for D14 bone marrow biopsy to detect residual disease when a morphologic blast cutoff of 20% or greater and bone marrow cellularity of 20% or greater is utilized. For those patients with residual blast counts over 20% and non hypocellular marrow, strong consideration should be made for clinical trial or novel therapeutic agent. Although these are relatively small numbers, this data underscores the continued value of D14 bone marrow morphologic assessment for prognostication.
Reagan: Teva: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract