Abstract
Acute myeloid leukemia (AML) is initiated and maintained by a relatively rare leukemia stem cells (LSCs) that are capable of self-renewing, proliferation and differentiation into leukemia blasts. Recent data showed that LSCs (Lagadinou et al. Cell Stem Cell 2013) and residual cytarabine (Ara-C)-resistant AML cells (Farge et al. Cancer Discovery 2017) are highly dependent on mitochondrial function for survival. This unique metabolic biology makes LSCs and AML cells resistant to chemotherapy vulnerable to oxidative phosphorylation (OXPHOS) inhibition. We have identified a novel potent inhibitor, IACS-010759, which blocks mitochondrial complex I, suppresses OXPHOS and selectively inhibits the growth of AML cells (Molina et al. AACR 2016). In this study, we aimed to determine the effects of OXPHOS inhibition with IACS-010759 on residual AML cells and AML LSCs surviving standard chemotherapy (Doxorubicin/Ara-C, DA) in patient-derived xenograft (PDX) AML models.
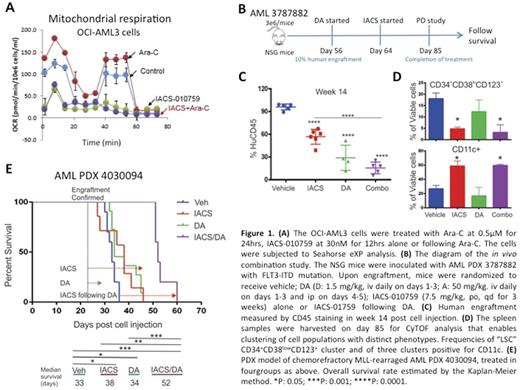
Consistent with Farge et al study, OCI-AML3 cells treated with DA in vitro produced elevated levels of reactive oxygen species, displayed increased mitochondrial membrane potential and higher mitochondrial mass (data not shown), indicating reliance on mitochondrial metabolism. Further, Ara-C facilitated statistically significant increase in the basal and maximal oxygen consumption rates (OCR) (36%±8%, p=0.03; 36%±3%, p=0.003, respectively) compared to control. In turn, OXPHOS inhibition with IACS-010759 at 30 nM fully inhibited basal and Ara-C-induced OCR (Fig. 1A). These findings indicate that chemotherapy fosters mitochondrial respiration in AML, which could be abrogated by OXPHOS inhibitor.
To examine the efficacy of IACS-010759 on residual leukemia cells surviving chemotherapy in vivo, we first established a chemosensitive PDX AML model of minimal residual disease. Treatment of mice inoculated with a human AML PDX harboring FLT3-ITD mutation with DA (D: 1.5 mg/kg; A: 50 mg/kg) reduced leukemia burden (PB, 0.8 ± 0.6% vs 45.8 ± 8.2% in vehicle-treated mice, p=0.001). The residual AML cells in DA-treated mice expanded and caused rapidly progressing leukemia (78.2 ± 6.2% vs 95.3 ± 1.0% in vehicle-treated mice, p=0.047) on week 6 post DA. Daily oral treatment of mice with IACS-010759 (7.5 mg/kg) as a single agent reduced leukemia burden, and caused further reduction when administered post completion of DA (Fig. 1B,C). The CyTOF mass cytometry, which enables measurement of up to 40 parameters per cell, demonstrated reduced frequency of CD34+CD38lowCD123+ AML LSCs and resurgence of CD11c+ differentiated cells in both IACS and IACS/DA groups (Fig. 1D). On the contrary, chemotherapy alone failed to significantly reduce fractions of LSCs or induce differentiation (Fig. 1D). Proliferation measured by Ki67 was greatly reduced by IACS/DA combination in all populations (1.4 ± 0.3% vs 5.5 ± 0.4% in vehicle group, p<0.01). The expression of hypoxia-inducible factor 1α was downregulated, consistent with the decreased oxygen consumption by IACS-010759 (not shown).
We next investigated the efficacy of IACS-010759 in a chemoresistant PDX model inoculated with chemorefractory MLL-rearranged AML. CyTOF analysis demonstrated that DA chemotherapy failed to reduce the primitive leukemia stem/progenitor populations, which comprised 84.7% of total cells in DA versus 71.2% in vehicle groups, while the combination of IACS-010759 and DA efficiently reduced this population down to 30.2%. Additionally, the combination increased the proportion of mature cells characterized by CD34-CD64+CD11b+ (43.1% versus 12.8% in vehicle), which remained low in the DA-only group (5.6%). DA/OXPHOS inhibitor combination significantly extended survival, compared to the vehicle or single-agent treatment arms (Fig. 1E).
In conclusion, AML cells surviving chemotherapy depend on OXPHOS for survival, and OXPHOS inhibition with complex I inhibitor IACS-010759 reduces AML LSC pool, induces differentiation and extends survival in AML PDX models in vivo . Our data advocate for combining IACS-010759 with standard chemotherapy, upon identification of a recommended Phase II dose in an ongoing clinical trial of IACS-010759 in AML (NCT02882321).
Battula: United Therapeutics Corporation: Research Funding. Andreeff: Daiichi Sankyo: Consultancy. Kantarjian: ARIAD: Research Funding; Delta-Fly Pharma: Research Funding; Amgen: Research Funding; Pfizer: Research Funding; Novartis: Research Funding; Bristol-Meyers Squibb: Research Funding. Daver: Karyopharm: Consultancy, Research Funding; Incyte Corporation: Honoraria, Research Funding; Bristol-Myers Squibb Company: Consultancy, Research Funding; Daiichi-Sankyo: Research Funding; Sunesis Pharmaceuticals, Inc.: Consultancy, Research Funding; Jazz: Consultancy; Otsuka America Pharmaceutical, Inc.: Consultancy; Pfizer Inc.: Consultancy, Research Funding; Novartis Pharmaceuticals Corporation: Consultancy; Kiromic: Research Funding; Immunogen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.