Abstract
Background: AML is an aggressive malignancy with a median age of 67 years at diagnosis and an age-adjusted 5-year (yr) survival of less than 25%. Most older patients (pts) with AML have poor risk cytogenetic/genetic features associated with a complete remission (CR) rate of 30-50% and a 5-yr overall survival (OS) probability of ~10%. Aside from the recent approval of midostaurin for FLT3-mutated AML, the induction strategy for the majority of intensive-chemotherapy eligible pts has remained unchanged for nearly 4 decades. Vosaroxin, a first-in-class anticancer quinolone derivative, administered in combination with intermediate dose cytarabine (IDAC) in relapsed/refractory (r/r) AML pts has demonstrated the ability to significantly improve CR rates compared to IDAC alone, and has a well described safety profile. As vosaroxin ± intermediate dose cytarabine has been successfully administered and tolerated in both pts of advanced age (≥ 60 years) and those with r/r AML, we have pursued investigation of the combination of infusional cytarabine with vosaroxin ("7+V") in newly diagnosed AML.
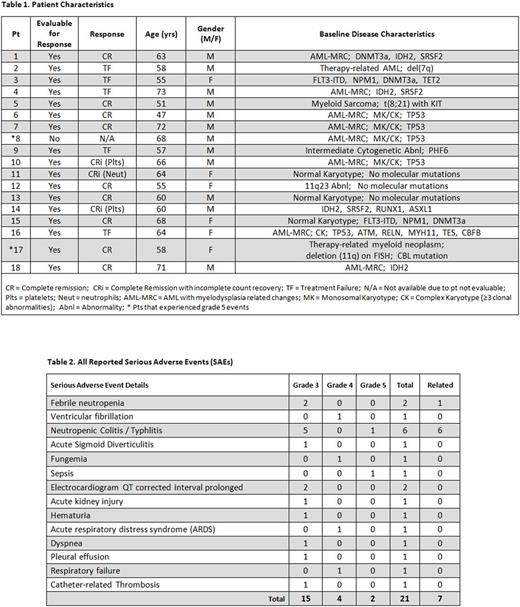
Methods: VITAL (NCT02658487) is a single-arm, open-label, Simon-like two-stage phase II study of 90 mg/m2 vosaroxin on days 1 and 4 (reduced to 70 mg/m2, days 1 and 4 in the event of re-induction) and 100 mg/m2 continuous infusion cytarabine on days 1-7. Oral cryotherapy was administered during vosaroxin administration as prophylaxis for oral mucositis seen in prior studies. Enrollment in stage 1 was limited to 17 evaluable patients with newly diagnosed untreated AML. In Stage 1, pts ≥ 55 yrs of any risk classification were allowed, while enrollment of pts aged 18-54 years was limited to patients with high-risk disease characteristics. The primary endpoint was CR rate. The two-stage design required CR in more than 7 of the first 17 pts in order to proceed to stage 2 and increase enrollment up to 41 pts by including an additional 24 pts and allowing pts 18 years and older with intermediate or high risk disease and those 55 years or older with any risk disease. The operating characteristics of the study design provided a 64% probability of early termination if CR occurred in 7 or fewer pts suggesting that the true CR rate would be 40% or lower. Response was assessed using the modified IWG-2003 criteria.
Results: In stage 1 of the trial, 18 pts were enrolled [Table 1]. One patient who achieved an aplastic marrow biopsy at day 14, succumbed to an AML related sepsis event prior to formal response assessment was deemed unevaluable and replaced. Of 17 evaluable pts, median age was 60 yrs (range, 47-73) and 88% (15/17) were ≥ 55 yrs at time of enrollment. Oral mucositis was observed in 6/17 (35%) pts with 3/6 having maximum grade (Grd) 1 severity and 3/6 having maximum Grd 3 severity. All reported serious adverse events (SAEs) are listed in Table 2. Five Grd 3 neutropenic enterocolitis SAEs related to protocol defined therapy occurred in stage I. Two Grd 5 events occurred: 1-sepsis (related to AML); 1-neutropenic colitis (related to protocol defined therapy). Of the 17 evaluable patients in stage I, CR was achieved in 9 pts (53%), while 3 additional pts achieved CR with incomplete count recovery (CRi) leading to an overall response (CR+CRi) rate of 71% (12/17). One pt with CRi (pt #10) converted to CR in the absence of additional therapy but did so outside of the protocol defined time period for response assessment (Day 57 +/- 3 days) and was recorded as CRi with respect to this analysis. CR was noted in 3/4 of the evaluable pts whose AML had TP53 mutations at diagnosis.
Conclusion: The combination of vosaroxin and infusional cytarabine in newly diagnosed AML pts appears safe with mucocutaneous complications observed that have been previously noted in studies of vosaroxin. The administration of oral cryotherapy during vosaroxin administration appeared to reduce occurrence of mucositis during induction. Neutropenic enterocolitis did occur at a rate consistent with standard induction chemotherapy but continues to be monitored closely. Altogether, the combination appears to be tolerable and the adverse event profile is similar to conventional induction regimens. While it is unclear if 7+V is superior to standard chemotherapy, the regimen is clinically active and the stage 2 portion of the trial continues to enroll. Response data, overall survival, disease-free survival, and data regarding ability to achieve transplant will be presented.
Strickland: Tolero: Consultancy; Boehringer-Ingelheim: Consultancy, Research Funding; CTI BioPharma: Consultancy; Novartis: Consultancy; Astellas: Consultancy; Sunesis: Consultancy, Research Funding; Baxalta: Consultancy. Podoltsev: Alexion: Consultancy; Ariad: Consultancy; CTI biopharma/Baxalta: Consultancy; Incyte: Consultancy. Zeidan: AbbVie, Otsuka, Pfizer, Gilead, Celgene, Ariad, Incyte: Consultancy, Honoraria; Takeda: Speakers Bureau; Otsuka: Consultancy. Stuart: Amgen: Consultancy, Honoraria; Bayer: Research Funding; Celator/Jazz: Research Funding; Pharmacyclics LLC, an AbbVie Company: Research Funding; Astellas: Research Funding; Agios: Research Funding; Novartis: Research Funding; Incyte: Research Funding; Sunesis: Consultancy, Honoraria, Other: Travel Support, Research Funding; Seattle Genetics: Research Funding; Cantex: Research Funding; MedImmune: Research Funding; ONO: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees. Savona: Incyte Corporation: Consultancy, Research Funding; Karyopharm: Consultancy, Equity Ownership; Celgene: Membership on an entity's Board of Directors or advisory committees; Gilead: Membership on an entity's Board of Directors or advisory committees; TG Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Sunesis: Research Funding; Amgen: Membership on an entity's Board of Directors or advisory committees; Takeda: Research Funding; Astex: Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.