Abstract
Background: Patients with lymphoma can be immunosuppressed from the disease, treatment or both. One indicator of cellular mediated immunity is reactivation of Varicella Zoster (VZV), a painful viral infection estimated to occur to 30% of U.S. population during a lifetime and associated with a particularly morbid post-herpetic neuralgia. Bortezomib and dexamethasone have been shown to be correlated with increased rates of varicella zoster and other viral infections (Kim SJ et al, Clinical lymphoma & myeloma, 2008). Autologous stem cell transplant depletes cellular- and humoral-immunity (Kamber C et al, BMT, 2015). While the main risk factor for VZV reactivation is age (Harpaz R, MMWR Recomm Rep, 2008), the underlying malignancy might play a large role in the risk of VZV reactivation. There is little data comparing the proportion of VZV in multiple myeloma (MM) with other indolent B and T-cell lymphomas. The purpose of this study is to compare varicella infection in MM patients with chronic lymphocytic leukemia (CLL), cutaneous T-cell lymphoma (CTCL), and follicular lymphoma (FL). Given that VZV is a relatively common infection in patients with MM, we hypothesized that varicella reactivation in MM patients occurs at a higher rate than in patients with CLL, CTCL, or FL.
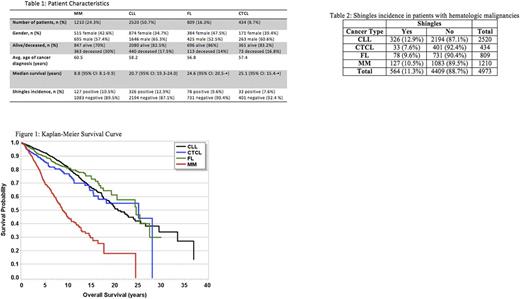
Methods: A retrospective chart review of 3,765 patients was conducted. Patients were eligible if they had been diagnosed with 1 of 4 malignancies - MM (1,210), CLL (2,520), CTCL (434), or FL (809). Patients diagnosed with other malignancies i.e. mantle cell lymphoma were excluded, as were patients with multiple malignancies i.e. MM and FL. All patients had been seen at the Ohio State University Wexner Medical Center during their treatment. For each patient, information on age, gender, length of survival, age at diagnosis of hematologic malignancy, and proportion of patients with shingles was collected. Only patients who were diagnosed with shingles after hematologic cancer diagnosis were included as positive. Associations between malignancy type and development of shingles were analyzed by a chi-square test, and logistic regression was used to calculate odds ratios for shingles between MM and the other malignancies, controlling for age as a possible confounder. Median survival time was calculated in years using the Kaplan-Meier method, calculated as the time from cancer diagnosis to date of last contact if alive, or date of death if deceased. Seven patients were excluded from survival analysis due to having the same date of diagnosis as date of last contact. This study was approved by the cancer institutional review board.
Results: Patient demographic information is found in Table 1. Of the 1,210 MM patients, 127 developed shingles after diagnosis (10.5%); of 2520 CLL patients, 326 were positive (12.9%); of 434 CTCL patients, 33 were positive (7.6%); of 809 FL patients, 78 were positive (9.6%). At a significance level of a=0.05, there was a significant association between cancer type and shingles (χ2=15.59, df=3, p-value=0.0014). Odds ratios comparing MM to each of the other lymphomas were not found to be significant. The median survival time in years was 8.8 for MM, 20.7 for CLL, 25.1 for CTCL, and 24.6 for FL (Figure 1).
Conclusion: Patients with MM had the lowest median survival (8.8 years), and a significant association between cancer type and shingle incidence was found, with CTCL patients having the lowest incidence of shingles (7.6%) within the retrospective period. However, the odds ratios comparing MM to the other 3 lymphomas was not significant, showing that the MM patients did not have significantly higher rates of shingles as originally hypothesized. These results demonstrate the differences in viral infection incidence and disease course between hematologic malignancies, and that antiviral strategies more specialized to T and B cell lymphomas may be important in reducing the risk of viral infection.
Hofmeister: Celgene: Research Funding; Adaptive Biotechnologies: Honoraria, Membership on an entity's Board of Directors or advisory committees; Karyopharm: Research Funding; Takeda: Research Funding; Thrassos: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Research Funding; Bristol-Myers Squibb: Research Funding; Roche: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.