Abstract

Objectives : Cancer Care Ontario (CCO) is the provincial governmental organization responsible for the planning of complex malignant hematologists (CMHs) in Ontario, Canada. The objective of this project was to estimate the need for CMHs in Ontario by developing a robust, data-driven method to estimate the average annual workload of a complex malignant hematologist for typical acute leukemia (AL) care.
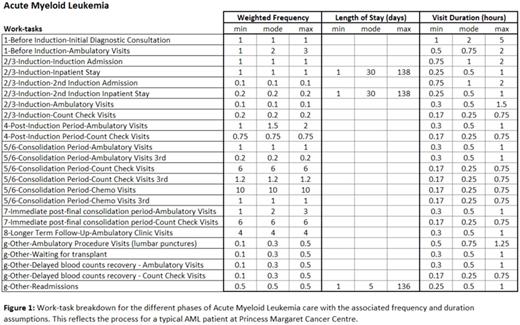
Approach : A detailed list of work-tasks (see Figure 1) was generated through clinical consultation to understand the patient/physician touchpoints involved in the typical care of patients with acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL). In the absence of data about the duration and frequency of each work-task, the clinicians estimated the minimum, mode and maximum duration and frequency for each of these work-tasks for a typical patient over their entire course of treatment. The average number of clinical hours available per CMH per year was also estimated. Data for inpatient length of stay as well as admission and readmission rates were derived from the Discharge Abstract Database from the Canadian Institute for Health Information. A Monte Carlo simulation was developed using these inputs to estimate the average workload of a CMH (# of new cases per CMH per year) for typical AL care. A triangular distribution using minimum, mode and maximum estimates was assumed for the simulation where historical data was not available. AL volume forecasts were modeled based on incidence and population demographics for the province. The average workload estimate was then used in combination with the AL forecasts to project the provincial need for CMH.
Results: From the results of the Monte Carlo simulation, typical AML and ALL patients require 43 and 89 hours of physician care per year, respectively, for a weighted average of 57 hours of physician care per year for the typical AL patient. An average of 1850 available hours per CMH per year for clinical work was estimated based on assuming 35-50 hours per week for clinical work (not including time spent on night/weekend call, billing administration, teaching, research or other non-clinical work) and 5 weeks of vacation with 10 days for statutory holidays. Combined, the workload benchmark was estimated at 32 AL new patients per year per CMH. With a projection of 727 new AL patients in Ontario in fiscal year 2016/17, this means that Ontario would need 22.7 dedicated CMHs to care for this cohort of patients.
Considerations: Due to the variability of duration of each work-task, the physicians found it very difficult to assign an average duration. The primary benefit of using a Monte Carlo simulation is that it allowed the physicians to state a range of durations rather than a point estimate of the average. This provided a more robust calculation of the workload along with increased confidence of the physicians in the outputs. In order to improve the estimates of duration for each of these work-tasks, a time-motion study can be used in the future to develop distributions of actual durations that can be inputted into the Monte Carlo simulation. If time spent on night/weekend call and non-clinical activities are considered, the number of CMHs required rises further and would be the subject of future work. Additionally, as this work focused on quantifying the need for CMHs providing AL care in Ontario, the provincial supply for CMHs was not specifically considered. Further work can be done to assess the current supply of CMHs who provide AL care and to model supply side issues such as retirement and recruitment.
Conclusion :Using a Monte Carlo simulation, we are able to estimate a workload benchmark of 32 new AL patients per year per CMH. This modelling paradigm can be used to estimate the AL CMH requirements in other jurisdictions where AL demand is known.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract