Abstract
The spleen is one of the few organs that can be entirely removed (or that can become severely dysfunctional) without major impact on immediate survival. In the long term however, splenectomised or asplenic patients are at risk of severe complications such as severe infections (mostly by encapsulated organisms), deep venous thrombosis, pulmonary embolism, solid tumor and hematologic malignancies (Sabatini 2011 Lancet, Jais Thorax 2005, Kristinsson Haematologica 2014). The spleen contributes to the efficient circulation of RBC in small vessels, a process essential for life. Stiff or sticky RBC are indeed cleared by the spleen before they would clog small vessels in other organs. We have previously shown that the deformability of RBC is mildly but significantly altered in splenectomised patients, even in those without preexisting RBC disease (Prendki et al. 2012). We hypothesized that loss of splenic filtration results in the presence in circulation of RBC subpopulations that could be associated with complications.
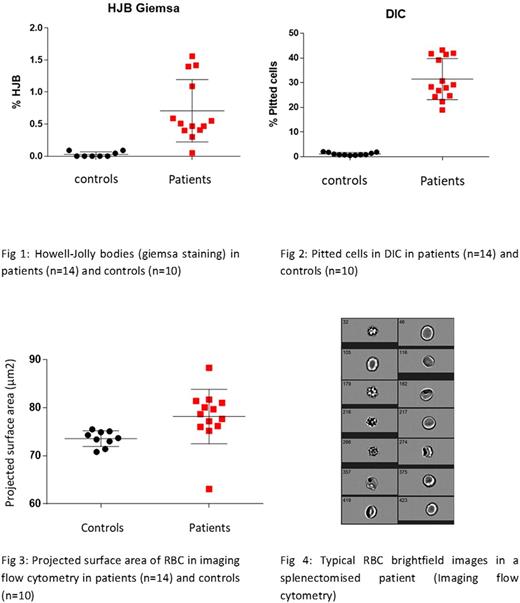
To explore this hypothesis, we assessed RBC morphology and deformability and markers of splenic function (pitted cells and Howell-Joly bodies) with a panel of reference tools and with innovative methods that we have developed (Buffet et al. 2006 ; Deplaine et al. 2011 ; Roussel et al. 2017) in 14 splenectomised patients and 10 healthy controls. RBC morphology and dimensions, numeration of pitted cells and of Howell-Joly bodies were assessed using imaging flow cytometry (AMNIS), differential interference contrast microscopy and blood smear. Deformability was determined by ektacytometry (LORRCA) and microsphiltration (Deplaine et al 2011). Reticulocyte count was done using cresyl blue and retic count.
The mean concentration of RBC containing Howell-Jolly bodies on Giemsa-stained smears was 0.71% (range 0.05-1.56) in splenectomised patients versus 0.03% (range 0-0.09) in controls (Fig 1). The mean concentration of RBC containing "pits" or vacuoles (pitted or pocked cells) visible with differential interference contrast (DIC) microscopy was 30.73% (range 18.94-43.24) and 1 % (0.48-1.52%) in patients and controls respectively (Fig 2). Imaging flow cytometry showed that splenectomised patients exhibit higher RBC projected surface area than do control subjects (Fig 3). Mean surface area was 78.18 µm2 (range 63.1-88.3) and 73.56µm2 in patients and controls respectively. This increase in surface area was associated with numerous morphological alterations in RBC including the presence of echinocytes, spheroechinocytes and spherocytes (Typical example is shown in Fig 4). These alterations were not observed in controls. Ecktacytometry confirmed the mild alteration of RBC deformability in splenectomised patients. Reticulocyte count showed no significative differences between patients and controls.
These observations confirmed that splenectomised patients exhibit morphological and deformability alterations that could contribute to complications (especially thrombo-embolic events). These alterations may also be new markers of splenic dysfunction and are currently been quantified in a larger number of patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.