Abstract
Introduction: Childhood anemia is a public health concern, particularly in India and in Africa, countries that account for 80% of the global burden. Usual treatment of childhood anemia in India consists of monthly distribution of Iron and Folic acid (IFA) tablets according to National Iron + Initiative guidelines. This approach is hampered in part by lack of anemia awareness, dietary practices, and poor adherence to IFA in the target population. To support anemia control efforts, we developed a novel community-centered education and counseling intervention optimized for delivery by village lay health workers (LHWs) to mothers of anemic children. The intervention consisted of five monthly sessions covering: a] anemia awareness education b] adherence counseling and assessment, c] dietary modification to improve iron intake, and d] hygiene and sanitation.
Methods: We evaluated the effectiveness of this intervention in a pragmatic cluster randomized controlled trial. Sixty villages selected at random from the study area in Karnataka, South India were randomly allocated to either intervention + usual anemia treatment (n=30) or usual anemia treatment alone (n=30). A cluster (randomization unit) was defined as a village from the study area together with its Anganwadi Daycare Center (ADC), and the corresponding LHW in charge of the ADC. LHWs in the intervention group were specifically trained to administer the intervention to mothers of anemic children in addition to usual anemia care. Hemoglobin at baseline and endpoint was used to define anemia (Hb<11gm/dl) and serum ferritin was used to define hypoferremia and iron deficiency anemia (IDA). Individuals with inflammation (elevated C - reactive protein) had the sTfR/log ferritin performed to diagnose IDA. The primary outcome of the trial was the difference in anemia cure rates between the experimental groups at the end of six months from the start of the intervention. Odds ratios of anemia cure were derived by logistic regression with the cluster design accounted for by random effects multilevel modeling.
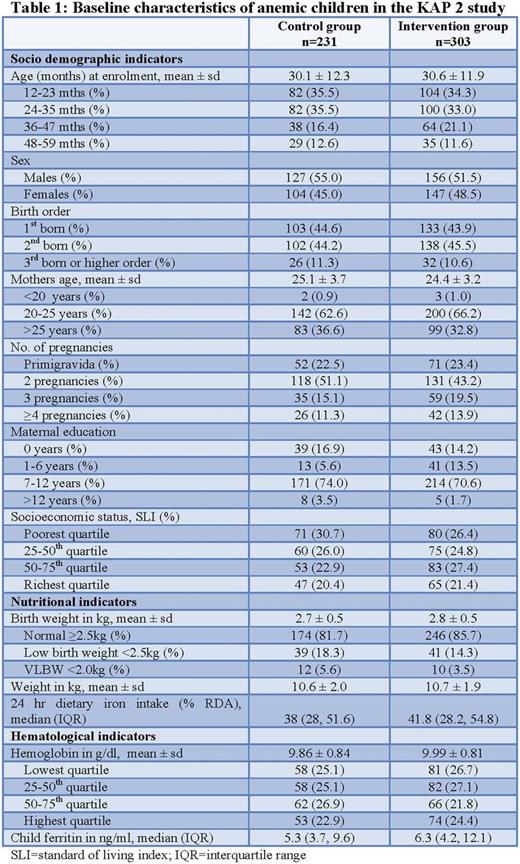
Results: From 55 finally included villages (intervention=28; control=27), a total of 1144 children were screened. The overall anemia prevalence was 47% (n=534; intervention=303; control=231). Baseline characteristics of the anemic children are presented in Table 1. Hypoferremia (ferritin<15ng/ml) was the predominant cause of anemia. In children with inflammation (hs-CRP>5 mg/L; n=55) all sTfR/log Ferritin values were >1.03 (median=2.7; 1.85, 4.20) suggesting functional IDA. Overall loss to follow up in the trial was low (3%) but was greater in the usual treatment group (n=12 vs. 5). According to an intention to treat analysis, children receiving the intervention had a significantly higher anemia cure rate compared with children receiving usual treatment (55.7% vs. 41.4%; p<0.001). A sensitivity analysis with best case scenario revealed at the very least a 12% difference in favour of the intervention group. Controlling for differences in maternal education and the child's baseline hemoglobin and weight, and taking into account the design effect, the probability of successfully curing anemia was 80% greater in the intervention than in the usual treatment group (OR = 1.8; 95% CI 1.07 - 3.02). The number of mothers needed to educate and counsel was 7 in order to cure one anemic child.
Conclusion: At the end of 6 months, the intervention combined with usual anemia treatment was more effective in curing anemia than usual treatment alone. This trial suggests that community education may positively interact with usual anemia treatment practices to achieve better childhood anemia control in India.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.