Abstract
Introduction: Mantle Cell Lymphoma (MCL) is an aggressive CD5-positive B-cell malignancy with a median survival of 3 to 5 years. A small subset of patients present with an indolent disease and can be managed on a "watch and wait" approach. Indolent MCL remains ill-defined, but is classically associated with hypermutated IGHV, non-nodal presentation, and absence of SOX11 expression. Up to 10% of MCL lack CD5 expression, but there has been limited attention given to its clinical and biological implications. We performed an extensive review of all reported cases of CD5-negative MCL to further characterize this disease subset.
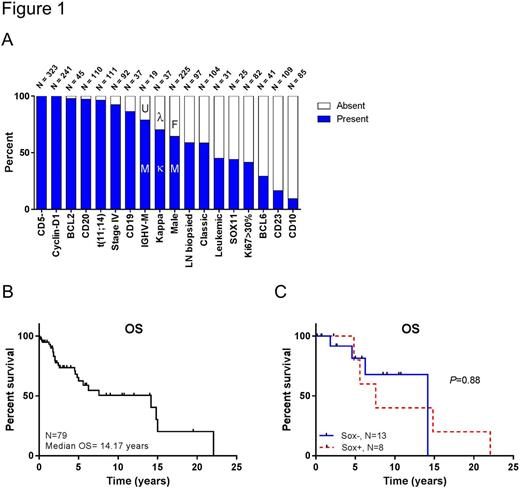
Patients and Methods: A systematic literature search was performed and included studies published from June 1994 to July 2017 in Pubmed, Embase, and Web of Science. We used the key words CD5 negative, CD5-, mantle cell lymphoma, and MCL. Data was tabulated regarding 20 variables: t(11;14)(q13;32), cyclin-D1, CD5, CD10, CD19, CD20, CD23, BCL2, BCL6, and Ki-67 (higher or lower than 30%), IGHV mutation status (mutated defined as >3% discordance with germline), SOX11, morphology, initial site of diagnosis, gender, age, light chain expression, presence of leukemic phase, stage, and overall survival (OS). Data was reported as percent and total number of cases with available data of each variable, and compared to historic data on CD5-positive MCL (referred to as conventional MCL). We used the Kaplan-Meier method to study OS, and log-rank test to compare OS between disease subsets.
Results and discussion: 140 of 818 screened articles included CD5-negative MCL cases. After exclusion of duplicates and non-English articles, 70 sources were included. Additionally, we included 2 cases identified at our institution. Data of 323 cases of CD5-negative MCL was collected (Figure 1A). Conventional and CD5-negative MCL shared certain similarities: both had a median age of diagnosis between 60 and 70 years, showed male predominance, and presented as stage IV disease. They shared overexpression of cyclin-D1 (100%, 241/241), possessed the t(11;14)(q13;32) (96%, 107/111: 107 of 111 cases with available data on translocation), were CD19-positive (86%, 32/37), CD20-positive (97%, 107/110), BCL2-positive (98%, 44/45), CD10-negative (91%, 77/85), CD23-negative (84%, 91/109), and BCL6-negative (71%, 29/41). Presence or absence of leukemic phase was reported in 31 cases, 14 of those were positive for circulating MCL cells (45%). Lymph node was frequently the initial site of MCL diagnosis (59%, 57/97). Majority of cases showed the classical MCL morphology with small to medium sized lymphoid cells (59%, 61/104). The proliferation marker Ki-67 was reported in 82 cases, 48 (59%) of which were <30%.
There were considerable clinical and biological differences between CD5-negative and conventional MCL. Most notably, the median OS (mOS) of 79 CD5-negative MCL cases with available follow-up was >14 years (Figure 1B), which compares very favorably to the historic survival of conventional MCL. SOX11, an MCL-specific biomarker that is positive in 90% of conventional cases was expressed in only 44% (11/25) of CD5-negative MCL cases. Lack of SOX11 expression in MCL predicts an indolent MCL subset. Surprisingly, OS was not significantly different between SOX11-positive and SOX11-negative CD5-negative MCL (Figure 1C, P=0.88). SOX11 stains were performed by expert hematopathologists at Tulane (2 cases) or other reliable institutions. Akin to SOX11 expression, λ light chain restriction and unmutated IGHV, two variables known topredict worse outcomes in conventional MCL, did not significantly impact OS in CD5-negative MCL. Similarly, higher Ki-67 expression (>30%) did not affect OS of CD5-negative MCL. Variables more prevalent in CD5-negative MCL compared to conventional MCL included κ light chain restriction (70%, 26/37) and IGHV hypermutation (79%, 15/19). Though sample size is limited, our survival analysis highly suggests that lack of CD5-expression might in fact represent an independently good prognostic marker in MCL.
Conclusion: Lack of CD5 appears to improve survival in MCL independently of other favorable prognostic markers such as IGHV hypermutation, absence of SOX11 expression, low Ki-67, and κ restriction. Reasons for this indolent behavior remain unknown. Our analysis indicates that CD5-negative MCL deserves deeper investigation to further understand its biological implications.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.