Abstract
Background: Malignant cells evade host immunity and change the milieu in the tumor microenvironment by activation of immune checkpoints, such as PD-1, PD-L1, PD-L2, and CTLA-4. Plasma cell myeloma (PCM) is one of the hematologic malignancies caused by immune dysregulation described as loss of effector T-cell populations and bone marrow (BM) microenvironment promoting immune escape. Though some investigators recently reported immune checkpoints in PCM, their results were controversial, and the application of immune checkpoints by means of treatment has not been clarified. In this study, we evaluated the expression of PD-1, PD-L1, PD-L2, and CTLA-4 in PCM patients according to disease course, genetic abnormalities and stages of Revised International Staging System (R-ISS).
Methods: We obtained 192 BM samples from 166 PCM patients (3 with R-ISS stage I, 37 with stage II and 17 with stage III) at Asan medical center in Korea between May 2016 and May 2017, including 85 at diagnosis and 107 after treatment, and normal BM samples were collected from 25 individuals with no evidence of hematologic malignancies as the controls. Expression percentages of PD-1 and CTLA-4 on T cells, and those of PD-L1 and PD-L2 on plasma cells and monocytes were measured using FACSCanto II (Becton-Dickinson, Sunnyvale, CA, USA) by flow cytometry.
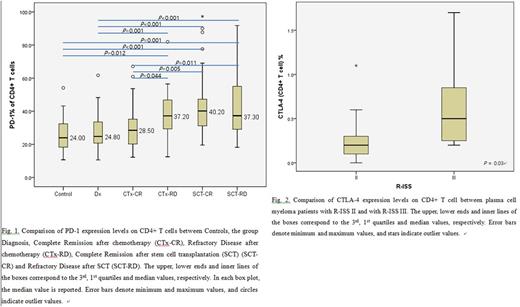
Results: At diagnosis, the median percentage of PD-1 expressed on CD4+ T cells was 24.8%, which shows no difference with that of the controls (Fig. 1). After stem cell transplantation (SCT) regardless residual disease, the expression levels of PD-1 on T cells were higher than those at the diagnosis (P < 0.001). The expression levels of PD-1 on CD4+ T cells in refractory disease after chemotherapy were significantly higher than in both of diagnosis (P= 0.001) and complete remission after chemotherapy (P= 0.044). CTLA-4 expression levels on CD4+ T cells positively correlated with the ratio of involved/uninvolved free light chain (P= 0.004, rho = 0.341). CTLA-4 expression on CD4+ T cell showed higher percentages in PCM patients with R-ISS stage III than those with R-ISS stage II disease (P= 0.03) (Fig. 2). Expression of PD-1 and CTLA-4 of CD4+ and/or CD8+ T cells showed higher values depending on the genetic abnormalities such as monosomy 13, 1q gain, complex chromosome and hypodiploidy. There was no meaningful tendency in the expression percentages of immune checkpoints on CD8+ T cells, on neoplastic plasma cells and on monocytes among PCM patients with different states.
Conclusion: We found that high expression levels of PD1 on CD4+ T cells associated with refractoriness against chemotherapy. We also found that PD-1 expression was upregulated by SCT and associated with several genetic abnormalities. The positive correlation between the expression levels of CTLA-4 on CD4+ T cells and R-ISS suggests that overexpression of CTLA-4 might depress anti-tumor host immune responses. We expect immune checkpoint blockades have therapeutic potential in refractory PCM patients after chemotherapy or SCT.
Lee: Boehringer Ingelheim: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.