Abstract
Background:
Multiple published studies have shown that abnormal coagulation tests, the prothrombin time (PT) and activated partial thromboplastin time (aPTT), are not helpful in predicting peri-operative bleeding. Despite numerous guidelines suggesting against their use, these tests continue to be ordered routinely in many pre-operative or pre-interventional settings.
Objective:
Our objective was to systematically assess the utility of unselected pre-operative PT and aPTT testing to predict bleeding outcomes.
Data sources:
We conducted a systematic literature review of MEDLINE, EMBASE and Evidence-based Medicine databases for articles published between 1970 and 2016 that addressed pre-operative and/or pre-interventional coagulation testing that was conducted in unselected fashion (i.e. not directed by the patient's personal/family history). Two independent reviewers (LL and AL) screened 3373 articles and 207 studies were included for full-text review.
Study eligibility criteria:
The minimum criteria for the 54 articles included in our qualitative analysis were: adult and/or pediatric patients undergoing elective surgery and/or an interventional procedure with pre-operative coagulation test results (PT and/or international normalized ratio (INR) and/or aPTT).
Outcomes:
The primary outcome was to examine the relationship between pre-operative coagulation results and peri-operative bleeding. As a secondary outcome, we also included studies that reported on the frequency of abnormal tests in routinely screened pre-operative patients as well as studies that described the cost of testing.
Results:
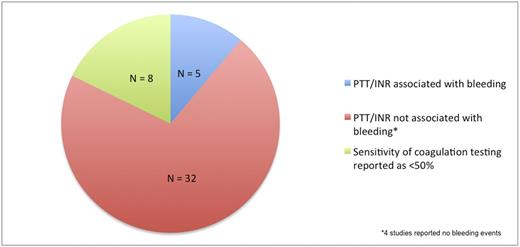
Of the 54 articles we included in our systematic review, studies were grouped according to procedure type: cardiac surgery (N=13), liver transplant (N=7) and tonsillectomy (N=13), major surgery (as defined in Choosing Wisely Canada, 2016) (N=12), and minor surgery (N=9). Within the combined studies of tonsillectomy and minor surgery categories, a total of 21 studies (after exclusion of 4 for insufficient data), there was only 1 study that showed an association between abnormal pre-operative coagulation testing and bleeding outcomes. Of the other 20 studies, 11 studies found no association between pre-operative coagulation studies and bleeding events, 4 studies had no bleeding events identified, 4 showed poor sensitivity of testing and 1 had no statistical information provided. In the major surgery category, there were a total of 26 studies (which included studies on liver transplant and cardiac surgery patients); only 4 studies identified an association between pre-operative coagulation testing and bleeding events, 17 found no association, and 4 described poor sensitivity of testing. In the studies that showed an association between pre-operative coagulation testing and bleeding, many used subjective definitions of bleeding, clinically insignificant thresholds to define abnormal aPTT and/or INR or provided insufficient data to support their conclusion. In summary, of the 45 studies with data on bleeding outcomes, the majority (71%) showed no association between bleeding events and pre-operative coagulation testing (Figure 1). As for assessment of quality, there were no randomized controlled trials (RCT) identified and the majority of observational studies were deemed at high risk of bias
Conclusion:
To our knowledge, this is the largest systematic review that assesses the utility of pre-operative coagulation screening as a predictor of perioperative bleeding. Of the 54 studies that met our eligibility criteria, only 5 showed an association between coagulation test results and perioperative bleeding. Our findings support current guidelines which caution against unselected pre-operative coagulation testing and also emphasize the need for a well-designed and powered prospective cohort study or RCT to definitively answer this important question.
Hicks: Gilead Sciences: Research Funding. Sholzberg: Octapharma: Honoraria, Research Funding; Shire: Honoraria, Research Funding; CSL Behring: Honoraria, Research Funding; NovoNordisk: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.