Abstract
Background: Autosomal dominant hyper IgE syndrome (AD-HIES) is a primary immune deficiency characterized by the classic triad of recurrent skin boils, cyst-forming pneumonias, and extreme elevations of serum IgE. AD-HIES is classically associated with mutations in the signal transducer and the activator of the transcription 3 gene (STAT3) gene. To date, the majority of cases have been caused by de novo pathogenic variants. The dedicator of the cytokinesis 8 gene (DOCK8) has been identified as the cause of many cases with autosomal recessive hyper-IgE syndrome (AR-HIES). The autosomal dominant hyper-IgE syndrome is associated with a cluster of facial, dental, skeletal, and connective tissue abnormalities which are not observable in the recessive type. Here we present a rare case of a patient meeting criteria for AD-HIES but with DOCK8 p.R83Q mutation.
Methods: Case study involving retrospective chart review from May 2015 to present.
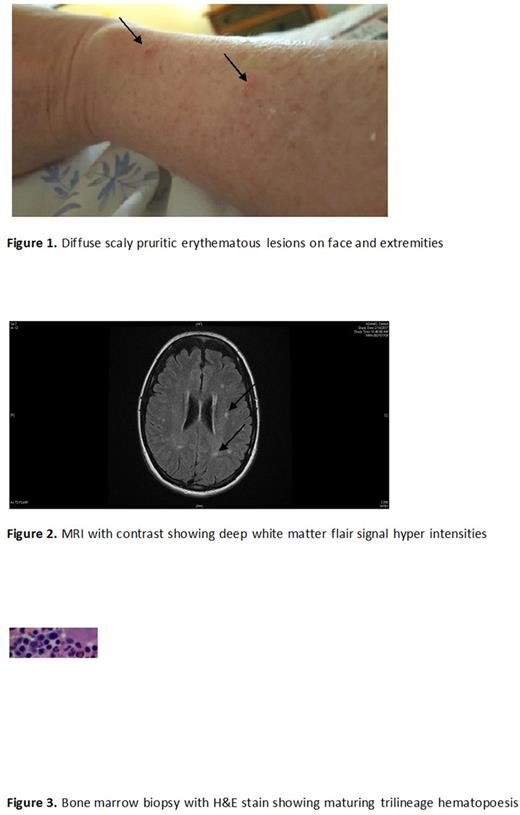
Clinical case: Patient is a 49 yo female with past medical history of moderate eczema, innumerable recurrent sinopulmonary infections, 4 episodes of pneumonia, mild scoliosis, 8 digital fractures with minimal trauma, 5 skin abcesses, recurrent vulvovaginal candidiasis, monthly urinary tract infections who presented to the emergency room in May 2015 with left facial paralysis and progressive paralysis in left upper and lower extremity associated with numbness. Physical examination revealed diffuse scaly pruritic rash, high palate, left facial droop, left sided upper and lower extremity weakness and numbness (Figure 1). MRI of the brain with contrast May 2015 showing scattered periventricular, subcortical and deep white matter FLAIR signal hyperintensities (Figure 2). CSF for viral, fungal, bacterial cultures, Cryptococcus, west nile, flow cytometry, protein electropheresis at that time was normal. She was found to have low IGG 579 mg/dL, normal IGA 191 mg/dL, IGM 111mg/Dl IGD 2.09 mg/dL, and increased IGE (297 IU/mL, currently 807 IU/mL, peak 1171 IU/mL). She had a complete negative workup for infections: Blood cultures, HIV, TB, EBV, CMV, HTLV-1&2, Colorado Tick Fever, Tropheryma Whipplei, Stongyloides, Schistosoma, Toxocara Abs, Ascaris, Plasmodium, Trichinella, Influenza A B, HSV, Hepatitis A B C, Echinococcues, West Nile virus, Cystercercosis, Lyme Disease, Syphilis, Amoebic cultures, Aspergillus, Mucormycosis. Stool was negative for ova & parasites, Shigella, Yersenia, Clostridium, Giardia, E. Coli, Trichome stain. Malignancy evaluation was negative including: CT brain, chest, abdomen, and pelvis, flow cytometry, protein electrophoresis, tumor markers, bone marrow biopsy and aspirate (figure 3), upper & lower endoscopy. Electrolytes, metal screen (arsenic, copper, lead, mercury, zinc), complete chemistries were negative. A complete autoimmune and allergy panel was negative. Immunology profile showed normal CBC (normal PLT size), low CH 50 of 38 U/mL, normal helper CD3% 78%, 1884 cell/mcL, elevated helper CD4% 68.5%, 1601 cell/mcL, low suppressor CD8% of 11% with normal absolute number 249 cell/mcL. IL 6 = 3.1 pg/mL, IL 10 =11.5 pg/mL, IL 12 was undetectable. Genetic analysis revealed normal NOTCH3, SPINK5, STAT3, TYK2 genes. A heterozygous mutation in DOCK8 p.Arg83Gln (R83Q) was discovered in this patient. Based on a clinical scoring system developed by the National Institutes of Health patient has features suggestive of AD-HIES (> 40 is cutoff, our patient scored 52). The patient has been receiving IVIG 40 grams IV every 3 weeks with clinical improvement in infectious symptoms but continued progression of neurological symptoms. Due to rarity of this case the patient is currently being referred to the NIH for further management.
Conclusion: Here we present a rare adult onset case with the patient meeting criteria for AD-HIES and symptoms of DOCK8 AR-HIES harboring R83Q variant DOCK8. This patient may likely harbor an undiscovered mutation in another allele.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.