Abstract
Background
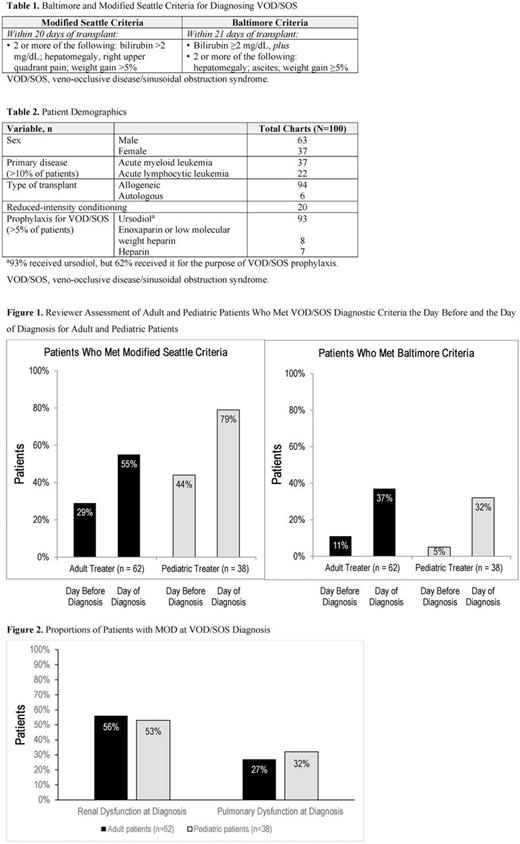
Hepatic VOD/SOS is a potentially life-threatening complication of conditioning for hematopoietic stem cell transplant (HSCT). VOD/SOS with multi-organ dysfunction (MOD) may be associated with >80% mortality. Historically, VOD/SOS has been diagnosed in pediatric and adult patients using either modified Seattle or Baltimore criteria, both of which include hepatomegaly, ascites, hyperbilirubinemia (included in modified Seattle criteria, but not required for diagnosis), and weight gain, within 20 to 21 days after HSCT (Table 1). The European Society for Blood and Marrow Transplantation recently proposed new criteria to facilitate timely diagnosis of VOD/SOS. Through a market research study, a retrospective chart review was conducted that examined VOD/SOS diagnosis patterns in a cohort of US physicians, including the timing of diagnosis and the presence of MOD at diagnosis.
Methods
Physicians each provided chart data for 1 or 2 patients with VOD/SOS who had received HSCT after April 1, 2016. Each physician completed a questionnaire form using the VOD/SOS patient's chart information; a chart reviewer checked the returned forms for completeness. A telephone interview was held with the physician to add any missing data. The participating physicians had diagnosed VOD/SOS per their discretion; criteria used for diagnosis were not recorded for this review; however, the objective measurements underlying the criteria were reported. For this analysis, chart reviewers assessed whether patients met modified Seattle or Baltimore criteria on the day prior to physician diagnosis of VOD/SOS and on the day of diagnosis. Time from suspicion of VOD/SOS to formal diagnosis also was collected for the subgroup of patients with MOD (renal and/or pulmonary dysfunction, per physician assessment) who later received VOD/SOS-specific pharmacologic treatment.
Results
A total of 63 physicians from 54 centers participated. Of these, 39 (62%) with an adult focus (adult treaters) provided 62 charts, and 24 (38%) with a pediatric focus (pediatric treaters) provided 38 charts. Among the 100 patients with VOD/SOS (Table 2), 83 had MOD.
Based on the reviewer assessment, 29% of adults and 44% of pediatric patients for modified Seattle, and 11% of adult and 5% of pediatric patients for Baltimore (Figure 1) met VOD/SOS diagnostic criteria 1 day prior to the physician's diagnosis. When the 20- to 21-day post-HSCT timeframe criterion was removed (clinical diagnostic criteria could be reached at any time after transplant), the percentage of patients who met criteria 1 day prior to physician diagnosis increased to 48% (adults) and 50% (pediatrics) for modified Seattle criteria, and 21% (adults) for Baltimore criteria (all pediatric patients were diagnosed by day 21).
Overall, 56% of adult and 53% of pediatric patients had renal dysfunction at VOD/SOS diagnosis; pulmonary dysfunction at VOD/SOS diagnosis was reported in 27% of adult and 32% of pediatric patients (Figure 2). In the subgroup of patients with VOD/SOS-related MOD receiving pharmacotherapy for VOD/SOS (n=52) the gap between physician suspicion and formal diagnosis of VOD/SOS (per questionnaire forms) was ≤3 days for 63.5% of patients and 4 to 23 days in 36.5% of patients (median = 2.5 days). Only 2 of 52 patients (3.8%) in this subgroup received a diagnosis of VOD/SOS on the day their physician first became suspicious of VOD/SOS.
Conclusions
On the day before diagnosis by the treating physician, 29% to 44% of patients met modified Seattle, and 5% to 11% met Baltimore diagnostic criteria for VOD/SOS, in this retrospective chart review collected through market research. There may have been an additional gap in diagnosis of VOD/SOS in the cohort of patients with MOD receiving VOD/SOS-specific pharmacotherapy. In adults, 56% and 27% had renal or pulmonary dysfunction, respectively, on the day of diagnosis. These groups were 53% and 32% in pediatric patients. A substantial number of patients presented with multi-organ involvement and met the clinical diagnostic VOD/SOS criteria beyond the 20- to 21-day timeframe post-HSCT. Limitations of this analysis include its retrospective nature, small sample size, subjectivity of physician definition of VOD/SOS and MOD, and potential confounders such as comorbidities and differences in VOD/SOS severity.
Support: Jazz Pharmaceuticals.
Del Pino: Jazz Pharmaceuticals: Employment, Other: stock options. Rustay: Jazz Pharmaceuticals: Employment, Other: stock options. Mamedov: Jazz Pharmaceuticals: Employment, Other: stock options.
Author notes
Asterisk with author names denotes non-ASH members.