Abstract
Background: In cancer patients, the development of autoantibodies against coagulation factors is a rare but a life-threatening bleeding disorder. Acquired hemophilia A (AHA) is the most common subset of the disorder and is caused by the inhibitory antibodies against coagulation factor VIII (FVIII) activity which can cause significant bleeding diathesis in those patients. Therefore, a prompt diagnosis is necessary for management of controlling the suppression of the inhibitor and the bleeding diathesis.
Aims: We conducted a systematic review to study the occurrence of FVIII inhibitors in cancer patients, particularly their clinical outcomes and treatment responses.
Methods: We performed an electronic search through March 31, 2017 with search terms "acquired hemophilia factor VIII inhibitor and cancer", "acquired hemophilia A" in PUBMED and EMBASE. Manuscripts with unavailable details, other coagulation factor inhibitors, hereditary cases and in other languages were excluded. The primary endpoint was measuring clinical response to treatments as defined by reduction of at least 50% in the baseline FVIII inhibitor level. Secondary endpoints were identifying early (defined a time to response ≤ 1.5 months from the initiation of therapy) vs. late responders to treatments and overall survival (OS) between responders and non-responders.
Results:
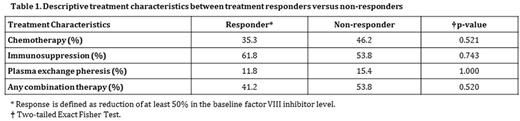
47 cases of AHA associated with malignancies were analyzed. Several cancer and hemophilia characteristics were compared between treatment responders and non-responders. Findings include 68% males, median age 70 (58-74), hematologic vs. solid malignancy of 62% vs. 38%, median FVII inhibitor level 14 BU/mL. The most common therapy used to eradicate the inhibitor was immunosuppressive therapy; differences in treatment modalities did not result in significant differences between responders and non-responders (Table 1). Treatment responders have lower median FVII inhibitor level as compared to non-responders (12 vs. 41 BU/mL; p = 0.027). There was equal number of cases for early and late responders. Median OS for responders was 41 months with 95 % CI [10.7-71.3] vs. 2 months for non-responders with 95% CI [1.3-2.7].
Conclusion:
The amount of inhibitor overall seems to be the best predictor of clinical outcomes in AHA patients regardless of the type of therapy used and the type of malignancy. Earlier detection of FVIII inhibitors could lead to earlier interventions with suppression therapy, potentially improving outcomes. Larger studies are needed to confirm our findings.
Rojas Hernandez: Daichii Sankyo: Research Funding. Oo: Daichii Sankyo: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.