Abstract
Background: Vaso occlusive crisis (VOC) is the most common reason for hospital admissions and emergency room visits in sickle cell disease (SCD). Education of patients, caregivers, and the healthcare team are a key factor in reducing readmission rates following hospitalization for children with VOC. There is a paucity of data on parental understanding of pain medications on hospital discharge, a confusing and intense time for families. This quality improvement (QI) project addresses provider and patient/parent knowledge gaps by incorporating a sickle cell pain action plan (SPAP) into the discharge process.
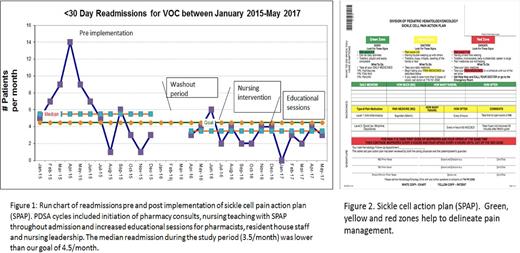
Objectives: The global aim was to decrease the 7 and 30-day readmission rates for VOC by 15% in a pediatric sickle cell population in one year. A multi-disciplinary team initiated a QI project at a single institution between April 2016 and May 2017.
Methods: The key drivers comprised of pharmacy, nursing, pediatric residents, patient representatives and pediatric hematologists. The SPAP was modeled on the success of the asthma action plan and helps distinguish patients degree of pain, with specific medical instructions for treatment. PDSA cycles included implementation of the SPAP with medication teaching at bedside, nursing teaching with SPAP during admission and pharmacy consults. The QI leader performed monthly educational modules to the house staff, pharmacists and nursing, and sent weekly email reminders to leaders of the inpatient team. Monthly run charts were created to assess 7 and 30- day readmissions. There are 14 months of data reported to capture both 7 and 30-day readmissions in the total study period. Readmissions were compared monthly to the year prior to implementation of the SPAP. Process measures were the number of documented pharmacy consults, documented SPAPs in the chart and surveys (5 point Likert scale) on patients understanding of their medications post discharge.
Results: There were 230 admissions for VOC the 12 months prior to implementation of the SPAP and 293 VOC admissions during the study period. Thirty-day readmission rates from April-July 2016 had a 36% reduction compared to 2015 data. The rise in readmissions during August, November and December of 2016 prompted implementation of new team champions and reeducation of staff, and subsequent months had reduction in readmissions. The cumulative decrease at completion of the project was an 18% reduction in thirty-day readmission rates and 13% reduction in 7-day readmission rates, whether or not there was a documented SPAP. Patients that had a documented SPAP in their chart (n=33) had a 65% reduction in thirty-day readmissions and 22% reduction in seven-day readmissions. Of the patients/parents surveyed (n=20 pre-implementation, n=34 post implementation) 91% and 74% strongly agreed they knew which pain medications to administer and how to escalate care compared to 56% and 47% prior to the project. Ninety percent of the surveyed families agreed that the SPAP: helped them understand their pain medications, remember medication names, was easy to understand and would be used again in the future. Pareto charts showed the following barriers to implementation of the QI intervention: pharmacy consults not performed due to lack of adequate staffing, SPAP documentation lacking despite a pharmacy consult being requested, and difficulties of staff adjusting to a new electronic medical record.
Conclusion: VOC readmission rates can be decreased by using a teaching tool to enforce medication understanding upon discharge. The SPAP was highly accepted in our patient population and empowered patients and families to treat their pain crisis at home once discharged.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.