In this issue of Blood, Yu et al used genetic barcoding of hematopoietic stem and progenitor cells (HSPCs) to study the impact of age on the hematopoietic reconstitution in primates and observe delayed emergence of multilineage clones and skewed hematopoiesis compared with younger controls. This experimental model represents a significant advance to study aged hematopoiesis.1
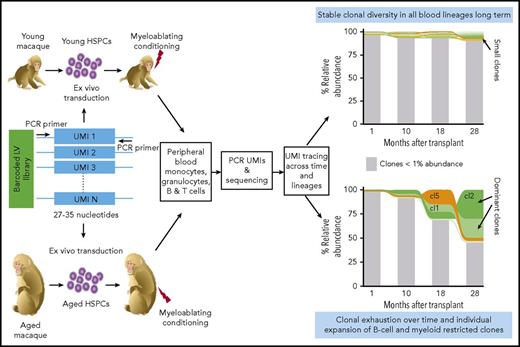
Clonal tracking of aged hematopoiesis by genetic barcoding in nonhuman primates. HSPCs from aged and young rhesus macaques are transduced with a GFP-expressing LV library containing unique molecular identifier (UMI) or barcode. Each LV-marked HSPC harbors a distinctive UMI stably integrated in its genome that will be inherited by its progeny after transplantation. Polymerase chain reaction (PCR) amplification and sequencing of the UMIs contained in the genomic DNA of peripheral blood–derived myeloid and lymphoid cells allows us to track and quantify clonal abundance of individual clones across time and cell lineages. The graphs on the right are a schematic example of the changes in clonal abundance and complexity over time in the blood of young and aged macaques; clones with an abundance >1% (cl1, cl2, and cl5) are color coded. Aged macaques display a reduction in clonal diversity and a pronounced expansion of both myeloid and B-cell lineage restricted clones at later time points compared with young macaques. The figure has been adapted from Figure 1 in the article by Yu et al that begins on page 1195.
Clonal tracking of aged hematopoiesis by genetic barcoding in nonhuman primates. HSPCs from aged and young rhesus macaques are transduced with a GFP-expressing LV library containing unique molecular identifier (UMI) or barcode. Each LV-marked HSPC harbors a distinctive UMI stably integrated in its genome that will be inherited by its progeny after transplantation. Polymerase chain reaction (PCR) amplification and sequencing of the UMIs contained in the genomic DNA of peripheral blood–derived myeloid and lymphoid cells allows us to track and quantify clonal abundance of individual clones across time and cell lineages. The graphs on the right are a schematic example of the changes in clonal abundance and complexity over time in the blood of young and aged macaques; clones with an abundance >1% (cl1, cl2, and cl5) are color coded. Aged macaques display a reduction in clonal diversity and a pronounced expansion of both myeloid and B-cell lineage restricted clones at later time points compared with young macaques. The figure has been adapted from Figure 1 in the article by Yu et al that begins on page 1195.
Aging in the hematopoietic system is characterized by reduced immune functions and increased tendency to develop anemia and malignancies. Functional and phenotypic changes in the HSPC compartment with age have been extensively characterized at the clonal level in mice. These studies reported that both cell-intrinsic and extrinsic stressors cause accumulating DNA damage and impair long-term tissue homeostasis of HSPCs.2 However, despite their value as indispensable tools for the interrogation of molecular determinants in normal and aged hematopoiesis, mice greatly differ from humans in size, life span, telomerase activity and proliferation capacity, and susceptibility to infection and/or oncogenic transformation.3 Conversely, studies of human aged hematopoiesis at steady state and upon transplantation are limited and mostly rely on the tracking of a small set of somatic mutations in blood cells as surrogates of clonal identity.4 Hematopoietic stem cell (HSC) gene therapy trials with integrating vectors allow tracing of hematopoiesis at the clonal level,5 but so far they have been carried out on pediatric patients precluding the possibility of studying the effects of aging on hematopoietic reconstitution. These limitations highlight the need to complement mouse and human studies on aging with humanized or more evolutionary related animal models.
Yu et al now provide an interesting approach of investigating the clonal output of young and aged HSPCs in the setting of autologous transplantation in rhesus macaques. In this study, 2 aged macaques (18 and 25 years old, corresponding to humans of 60-80 years) and 3 young animals (between 3 and 5 years of age) were transplanted with autologous CD34+ HSPCs transduced ex vivo with a GFP-expressing lentiviral (LV) barcoded library. Each LV genome contains a stretch of random nucleotides, known as “unique molecular identifier” or “barcode”; upon transduction, individual barcodes are stably inherited by the HSPC progeny during hematopoietic reconstitution.6 High-throughput sequencing of the genetic barcodes present in myeloid and T and B cells from peripheral blood harvested at different time points posttransplant allowed the quantitative study of the clonal output, clonal size, and multilineage potential of thousands of hematopoietic cell clones. The authors reported that in the initial months after transplant, HSPC contribution to both B-cell and myeloid lineages was comparable between young and aged animals, whereas the appearance of T cells was delayed in the aged group. Importantly, in both aged animals a progressive reduction in clonal diversity and a pronounced expansion of both myeloid and B-cell lineage restricted clones at later time points were observed when compared with younger counterparts (see figure).
Although the strategy used in this work represents a valuable advancement in studying aged hematopoiesis at the clonal level, some outstanding questions remain unanswered and require future investigations. For example, it is unknown whether aged macaques already had signs of oligo/clonal hematopoiesis or hematopoietic decline at steady state. One possibility is that the observed clonal output of aged HSPCs upon transplantation reflects age-associated changes in lineage composition of the infused cellular products. Indeed, pretransplant aged samples may be enriched in short-term HSCs or multipotent progenitors responsible for initial phases of hematopoietic reconstitution and depleted for long-term HSCs that should sustain hematopoiesis later on. As HSCs can only sustain a limited number of cell divisions throughout life before exhaustion,7 the proliferative history of HSPCs further exacerbated by the replication stress imposed by cell transplantation may contribute to the loss of clonal complexity with age. Moreover, it is unclear whether old macaques accumulate recurrent somatic mutations in genes such as DNMT3A, TET2, ASXL1, or JAK2, which are found in the blood of elderly human subjects at highly significant levels.4 Whole exome or genome sequencing data of the infused cells prior to and after transplant coupled with integration site analyses on populations and isolated cell clones are needed to further elucidate whether the observed clonal dynamics in aged macaques associate with selection of regulators/pathways that drive clonal hematopoiesis.
Another intriguing aspect will be to understand the underlying mechanisms by which aged HSPC clones are lost over time upon transplantation. Apoptosis and/or cell senescence, a permanent cell cycle arrest of damaged cells, may represent cellular outcomes responsible for intrinsic defects of the regenerative capacity of aged HSPCs.8 This hypothesis can now be tested given the reliability of molecular markers to detect senescent cells.9
The negative impact of aging on hematopoiesis is also modulated by extrinsic factors produced by the bone marrow niche.10 The use of autologous transplantation as employed by Yu et al did not permit dissecting the non–cell autonomous contribution of the microenvironment to aged hematopoiesis. However, as older subjects are eligible for allogeneic hematopoietic stem cell transplantation it will be important to study clonal dynamics in allogeneic transplantation settings in macaques in order to assess whether a younger host may revert the observed clonal output of aged HSPCs.
Although studying aged hematopoiesis in macaques will certainly allow delving deeper into the biology of aging of the hematopoietic system, there are also some limitations in the proposed model. Because of ethical, handling, and cost constraints, studies in nonhuman primates are executed on an extremely limited number of animals, thus reducing the power of the statistical analyses. Different HSPC mobilization protocols or cell doses at transplant could also have an impact on the repopulation dynamics and complicate the interpretation of the results. Furthermore, the clonal outputs during homeostatic turnover of old HSPCs cannot be addressed with the present settings that involve cell transplantation.
Despite all caveats, Yu et al define for the first time in primates the kinetics and lineage reconstitution at clonal level of aged HSPCs in autologous transplantation and provide a valuable approach for gaining mechanistic insights into the biology of the hematopoietic system and to experimentally test therapeutic strategies for aging and age-associated disorders.
Conflict-of-interest disclosure: The authors declare no competing financial interests.