Abstract
Background: Ischemic stroke is a cause of morbidity and mortality in children and adults with sickle cell disease (SCD). Recent studies showed that non-classical monocytes may be protective against vaso-occlusive crisis. Monocyte subsets have been examined in non-SCD stroke, but little is known about the role of monocyte or their subsets in ischemic stroke in SCD. CD64 (FCγRI), a high affinity receptor for IgG, is a marker of endothelial adherence on immature neutrophils in SCD, however it is more classically exhibited on activated pro-inflammatory monocytes. We hypothesized that higher levels of CD64 mean fluorescence index (MFI) on monocyte subsets may be associated with ischemic stroke due to increased adherence.
Methods: Adults (age ≥18) who presented for regularly scheduled clinic visits were enrolled. Blood samples were taken when subjects were at their healthy baseline and sent for complete blood count with differential. Monocytes were analyzed by flow cytometry and subsequently sub-classified by their CD14 and CD16 expression into classical (CD14high, CD16 low), intermediate (CD14high, CD16high), and non-classical (CD14low, CD16high). The CD64 MFI was determined for each monocyte subset. History of ischemic stroke was confirmed by neurologist or neuroimaging documentation in the medical record. Laboratory results between those with a history of stroke and those without history of stroke were compared using Student's T Tests. We modeled log-odds of stroke history for increasing levels of each monocyte subtype and CD64 MFI using both marginal and age-adjusted multivariate logistic regression.
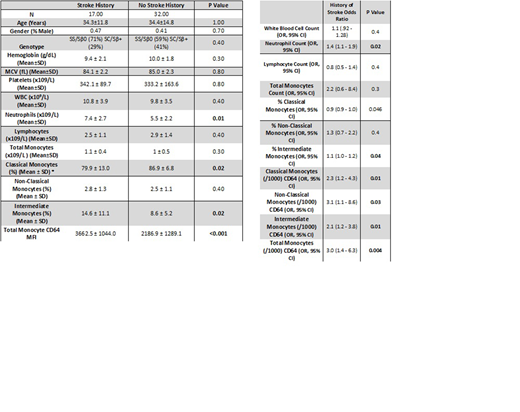
Results: We enrolled 49 adults, of whom 17 (35%) had a history of ischemic stroke. There was no difference in age, gender, or genotype between the two groups (Table 1). Patients with a history of stroke had higher total neutrophils, but there was otherwise no difference in complete blood counts (Table 1). When monocyte subsets were examined, patients with a history of stroke had a higher percent of intermediate monocytes and a lower percent of classical monocytes (Table 1). Patients with history of stroke also had a higher MFI (mean fluorescence index) both overall and on each monocyte subset. (Table 1). In univariate models increased levels of classical monocytes were associated with decreased odds of stroke history and increased levels of intermediate monocytes, CD64 MFI on each monocyte subtype, total monocyte CD64 MFI, and total neutrophil count were all associated with increased odds of stroke history (Table 2). However, in multivariate models adjusted for age and monocyte subtype percent only total monocyte CD64 MFI and total neutrophil counts remained significant and both had increased odds ratios for ischemic stroke history, (OR 3.8 per 1000 CD64 95% CI 1.2 - 11.4, p= 0.02, OR 1.2 per 1x10^9/L 95% CI 1.0 - 1.4, p=0.05 respectively, R-squared 0.45).
Conclusion: Levels of monocyte subsets have been shown to correlate with clinical outcomes in non-SCD stroke, but to our knowledge this is the first study to examine their roles in ischemic stroke in SCD. The pathophysiology of stroke in SCD is unique and the role of monocytes in it deserves separate study from the role of monocytes in non-SCD stroke. We saw that while monocyte subsets were associated with a history of ischemic stroke, CD64 MFI on all monocyte subsets showed a strong association. We wonder if this may be due to CD64 MFI being a marker for cells which are more adherent to endothelium as has been shown in previous studies. This creates a need for future studies. In particular it would be valuable to know if increased CD64 MFI precedes stroke and could be used as a marker of future stroke risk.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.