Abstract
Background: Monosomy of chromosome 7/Del 7 (-7) or its long arm (del(7q)) is one of the most common cytogenetic abnormalities in pediatric and adult myeloid malignancies, particularly in adverse-risk acute myeloid leukemias (AMLs). Monosomy 7 with complex karyotype further worsens the prognosis. Therefore, predicting response of therapies in this segment of patients is urgently needed to improve disease management by customizing therapy to the profile genomics instead of the conventional method of trial and error or one-size-fits all treatments.
Aim: Predictive analysis of disease characteristics of Monosomy 7 and Sub-clustering of this segment along with identification of therapy options for treatment of this cohort using computational biology modeling (CBM).
Methods: We selected a cohort of 1168 AML patients whose genomics and clinical data was collated from public domain datasets and literature. Using CBM, patients with (-7) were identified from this larger cohort and were sub-clustered using a machine learning approach.
The genomic data of the representative patients per sub-cluster of (-7) cohort were used to generate disease-specific protein network maps. Digital drug simulations were done by quantitatively measuring drug effect and calculating a disease inhibition score (DIS) that is a composite of proliferation, viability and apoptosis along with impact on disease specific biomarker score. Each patient-specific map was digitally screened for the extent by which standard of care (SOC) and combinations with Non-SOC inhibited the disease.
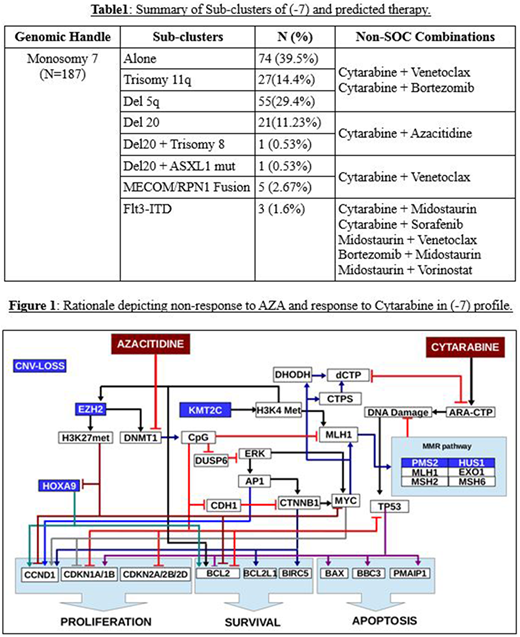
Results: CBM identified 187 (-7) patients (16%) that grouped into 8 sub-clusters (Table 1). CBM analysis of genomics of each sub-cluster representative identified combination therapy options for this cohort with poor response to SOC, supported by genomics driven disease characteristics.
Monosomy 7 aberrations would lead to decreased expression of EZH2, CARD11, EIF3, PMS2, HUS1, KMT2C (MLL3), CDK5 and IKZF1. Azacitidine (AZA) is predicted to be a non-responder in this cohort due to decreased expression of EZH2, that would impact DNA methylation via reduced recruitment of DNMTs. Lenalidomide (LEN) is also predicted to be a non-responder due to decreased expression of IKZF1, CARD11, and EIF3 despite presence of Del5q, a strong inclusion for LEN response.
This segment has shown high microsatellite instability (MSI) characteristics and this could be linked to reduced mismatch repair (MMR) pathway due to reduced expression of PMS2, HUS1 and KMT2C. This characteristic could explain certain patient cases with (-7) who have responded to Cytarabine. (Figure 1) However, the response rate of chemotherapy in (-7) cohort is <50% and relapse is high. (PMID 12393746) Loss of histone methyltransferase EZH2 through reduction of H3K27 trimethylation can be the key reason for inducing resistance to many AML cytotoxic drugs.
With (-7), CBM analysis determined an increased expression of BCL2 due to reduced methylation and HOXA9 expression. (PMID: 9562974) Proteasomal subunit PSMB5 gets down regulated due to CDK5 loss which would make the cohort more sensitive to proteasomal inhibition. This can also help with controlling EZH2 levels in the disease via regulating EZH2 proteasomal degradation. (PMID: 21289309, 27941792) CBM predicted that a combination of Cytarabine + Bortezomib and Cytarabine + Venetoclax could be effective in the (-7) AML cohort.
Conclusions: CBM analysis of AML patient genomics identified abnormal protein networks and drug resistance pathways in patients with monosomy 7, and combination therapy options in the (-7) sub-clusters. EZH2 was identified as a key reason for resistance and combinations of Cytarabine with proteasome or BCL2 inhibitor was predicted to be effective in this cohort.
Vali:Cell Works Group Inc.: Employment. Cogle:Celgene: Other: Steering Committee Member of Connect MDS/AML Registry. Singh:Cellworks Research India Private Limited: Employment. Usmani:Cellworks Research India Private Limited: Employment. Pampana:Cellworks Research India Private Limited: Employment. Shyamasundar:Cellworks Research India Private Limited: Employment. Sikora:Cellworks Research India Private Limited: Employment. Kumar:Cellworks Research India Private Limited: Employment. Abbasi:Cell Works Group Inc.: Employment.
Author notes
Asterisk with author names denotes non-ASH members.