Abstract
Background: Sepsis-associated disseminated intravascular coagulation (DIC) is a complex clinical scenario involving derangement of many processes, including hemostasis. Assessment of markers of these other aspects of disease, including inflammation, immunity, endothelial function, and endogenous anticoagulants may provide insight into DIC pathophysiology and lead to improved methods for assessment of patient condition and response to treatment. This study was designed to measure biomarkers representative of multiple systems involved in DIC development in a cohort of patients with sepsis and DIC and determine the association of these biomarkers with disease severity and mortality.
Materials and Methods: Citrated plasma samples were prospectively collected from 102 patients with sepsis and suspected DIC at ICU admission (day 0) and again serially on ICU days 4 and 8 under an IRB approved protocol. DIC score was determined using the ISTH scoring algorithm (e.g. platelet count, PT/INR, fibrinogen, and D-Dimer). Plasma from healthy individuals was purchased from a commercial laboratory (George King Biomedical, Overland, KS). . CD 40 Ligand (CD40L), Plasminogen inhibitor 1 ( PAI-1), nucleosomes, Procalcitonun (PCT), Microparicle Tissue Factor (MP-TF), and Prothrombin Fragment 1.2 (F1.2) were measured using commercially available ELISA kits. Protein C activity was measured using a clot-based assay. Interleukin 6 (IL-6), Interleukin 8 (IL-8), Interleukin 10 (IL-10) , Tumor Necrosis Factor Alpha (TNFα) , Monocyte Chemoattractant protein 1 (MCP-1) were measured using a biochip technology.
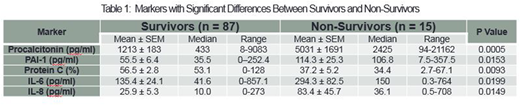
Results: Significant differences in levels of Protein C (p=0.009), PCT (p=0.0005), IL-6 (p=0.019), IL-8 (p= 0.015), and PAI-1 (p=0.015) were observed between survivors and non-survivors (Table 1). Significant variation of Protein C (p=0.002), nucleosomes (p=0.05), PCT (P<0.001), IL-6 (p=0.001), IL-8 (p=0.003), IL-10 (p=0.011), TNFα (p=0.021), and MCP-1 (p=0.21), were observed based on severity of DIC score.
Conclusion: Markers from multiple systems perturbed in DIC were associated with mortality suggesting that while these systems may not be routinely evaluated in the course of patient care, dysfunction of these system contribute significantly to mortality. In addition, numerous inflammatory cytokines showed an association with DIC score. This study suggests that the measurement of additional markers in sepsis-associated DIC may be of value in the prediction of mortality and may be helpful in guiding treatment for these patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.