Abstract
Introduction
Acute myeloid leukemia (AML) is a heterogeneous disease that depends on precise risk-stratification for predicting outcomes and optimizing therapy plans. Despite the current clinical landscape of incorporating karyotype and mutations into prognostic models, chemosensitivity (or lack thereof) is usually not evaluated or appreciated until a patient undergoes a day 14 bone marrow (D14BM) evaluation during induction treatment. While the D14BM aspirate and biopsy are regularly used to predict achievement of CR versus need for further reinduction therapy, some have questioned its utility. Further, the invasive nature of the procedure leads to significant patient discomfort, anxiety, increased risk of complications (infections, bleeding, damage to surrounding tissues) and, at times, is not feasible due to a patient's critical state. Therefore, alternative criteria are needed to help risk-stratify these patients and predict treatment responses. We report here a single center analysis of the relationship between the rate of peripheral blood blast (PBB) clearance with cytotoxic induction therapy and clinical outcomes.
Methods
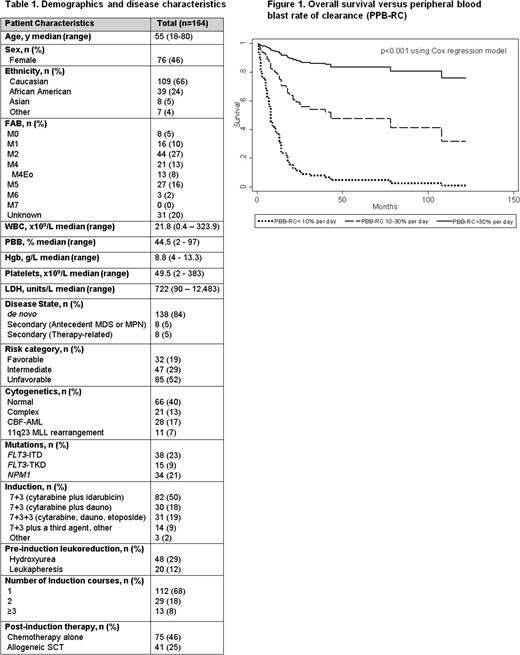
Patients diagnosed with AML (non-M3) with detectable PBB via manual differential or flow cytometry at University of Maryland Greenebaum Comprehensive Cancer Center (UMGCCC) during 2007-2018 were identified. Only patients who underwent induction with a "7+3" regimen with cytarabine and an anthracycline (idarubicin or daunorubicin), or "7+3" plus a third agent, were included. Patient and disease characteristics, treatment courses, and clinical outcomes were collected. The absolute PBB count was calculated by percent PBB multiplied by total leukocyte count (103/mcL). PBB rate of clearance (PBB-RC) was defined as the percentage of the absolute PBB count at diagnosis that was cleared each day, on average, until clearance or D14 of induction chemotherapy. Patients were divided into three groups based on PBB-RC: high, if PBB-RC >30% (n=15); low, if PBB-RC <10% (n=16); and intermediate, if PBB-RC fell between 10-30% (n=133). Primary outcomes included D14BM status, achievement of complete remission (CR) with or without full count recovery, and overall survival (OS). Multivariate logistic regression and Cox proportional hazards models were conducted and adjusted for the disease risk category, age, sex, ethnicity, and use of leukapheresis or hydroxyurea. Cox models were also adjusted for allogeneic stem cell transplantation (SCT) status.
Results
Treatment-naive AML patients with PBB at diagnosis and who underwent cytotoxic induction therapy were identified (n=164). Patient characteristics are shown in Table 1. Sixty-eight percent of patients underwent induction with "7+3", and 28% with "7+3" with a third agent. Pre-induction leukoreduction included hydroxyurea (29%) and/or leukapheresis (12%). Most (68%) patients received only one course of induction; 18% received 2 courses, and 8% received ≥3. Chemoablation on D14BM was achieved in 70% of patients (n=113); 27% (n=45) had residual disease, and 4% (n=6) were indeterminate. CR was achieved in 74% of patients (n=121), 19 of which required ≥ 2 induction courses. Forty-one patients proceeded to SCT. Median OS was 18.5 months (range 0.5-122).
Each 5% increase in PBB-RC approximately doubled the likelihood of D14BM clearance (OR=1.97; 95% CI: 1.39-2.80, p<0.001). The adjusted area under the ROC curve of PBB-RC for predicting D14BM clearance was 0.72, with a positive predictive value (PPV) of high PBB-RC of 93% and negative PV (NPV) of low PBB-RC of 81%. PBB-RC was also significantly associated with CR (OR per 5% =2.08; 95% CI: 1.38-3.14, p<0.001). CR was achieved in all patients in the high PBB-RC group, while only 44% in the low PBB-RC group. PBB-RC was significantly associated with improved OS (HR per 5%=0.67; 95% CI: 0.52-0.85, Figure 1). Other factors associated with longer OS included favorable risk category (HR=0.03; 95% CI: 0.01-0.23) and SCT (HR=0.50; 95% CI: 0.26-0.95). African American patients had poorer OS adjusted for PBB-RC (HR=2.22; 95% CI: 1.16-4.25), while race was not associated with D14BM or CR rate.
Conclusion
PBB-RC during induction chemotherapy is predictive of achievement of CR and improved OS in AML. PBB-RC is also significantly associated with D14BM clearance and can therefore serve as a surrogate predictive marker for treatment response in AML patients with PBB at diagnosis.
.
Emadi:NewLink Genetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.