Abstract
Background:
Polycythemia vera (PV), essential thrombocytosis (ET), and myelofibrosis (MF) are chronic myeloproliferative neoplasms (MPNs) characterized by clonal cell proliferation, splenomegaly, and significant symptom burden. Integrative medicine interventions may offer unique symptom management strategies. (Gowin, et al., EHA 2017). Here we describe integrative interventions utilized and association with symptom burden, quality of life, depression, and fatigue adjusted for lifestyle confounders.
Methods:Patients were recruited via social media. Consent and online self-report surveys were completed capturing patient demographics, disease-specific data, integrative medicine utilization, symptom burden via MPN-Symptom Assessment Form Total Symptom Score (MPN-SAF TSS), depression screening via Patient Health Questionnaire (PHQ)-2, fatigue via Brief Fatigue Inventory (BFI), and overall quality of life (QoL). MPN-SAF TSS, QoL, BFI, and PHQ2 were compared by participation in the most frequently utilized interventions (Yes vs No). Intervention comparisons were adjusted for alcohol consumption, smoking status, BMI, current dietary modification, and MPN type using multiple linear and logistic regression.
Results:
Patients:
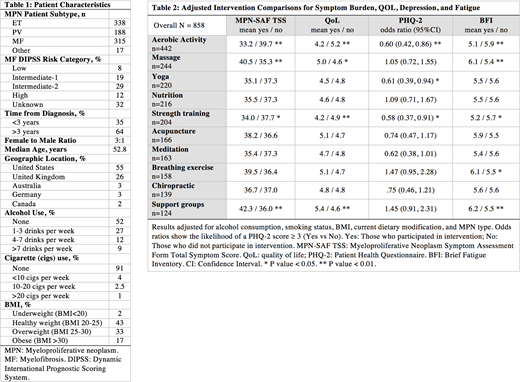
A total of1087 patient surveys were consented. Of these, 858 had 10 or more responses. See Table 1 for patient characteristics.
Integrative Medicine Therapies Descriptive Analysis:
Integrative medicine therapies most frequently utilized by patients included aerobic activity (51.5%), massage (28.4%), yoga (25.6%), nutrition (25.2%), strength training (23.8%), acupuncture (19.3%), meditation (19%), breathing exercises (18.4%), chiropractic (16.2%), support groups (14.5%), mindfulness based stress reduction (13.6%), walking meditation (12.0%), pet therapy (9.4%), aromatherapy (8.6%), music therapy (8.0%), progressive muscle relaxation (7.0%), guided imagery (6.4%), homeopathy (6.3%), manual therapy (osteopathy/cranial sacral) (6.2%), reiki (5.8%), therapeutic touch (5.7%), Tai Chi (5.2%), art therapy (4.9%), traditional Chinese medicine (4.3%), Qigong (3.5%), cooking classes (3.0%), laughter therapy (2.9%), Ayurveda (2.4%), biofeedback (2.2%), dance therapy (2.1%), hypnosis (2.0%), resilience training (0.9%), IV vitamin therapy (0.8%), and narrative medicine (storytelling) (0.3%).Diet modification was reported in 47.7% of patients, including Mediterranean diet (19.0%), paleo/high protein/low carbohydrate (8.9%), vegetarian (8.6), plant based (5.2%), gluten free (5.2%), low FODMAP (1.8%), vegan (1.2%), and raw (0.6%) diets. Only 24% of patients reported receiving nutrition advice from their healthcare practitioner (HCP).
Supplement utilization by MPN type was 162 patients (48.4%)in ET, 80 patients (42.8%) in MF, and 142 patients (45.2%) in PV. Overall, 20.6% patients reported not disclosing their natural product usage to their HCP. The most frequently utilized supplements included vitamin D, multivitamin, magnesium, omega 3, and calcium.
Adjusted symptom association with integrative therapy intervention:
MPN symptom burden: Aerobic activity (P=<.001)and strength training (P=.01) was associated with lower mean symptom burden. Use of massage (P=<001) and support groups (P=<.001) was associated with higher levels of symptom burden.
QOL:Higher quality of life was reported in those receiving massage (P=.04)and support groups (P=.002). Lower quality of life was noted in those using aerobic activity (P=<.001)and strength training (P=.001).
Depression (PHQ-2):Lower depression screening score was noted in those participating in aerobic activity (P=.006), yoga (P=.03), and strength training (P=.02).
Fatigue (BFI):Lower fatigue was noted in those participating in aerobic activity (P=<.001) and strength training (P=.03). Higher fatigue was noted in those participating in massage (P=<.001) and breathing techniques (P=.02). See Table 2.
Conclusion:
In a geographically diverse MPN patient population, and when adjusting for healthy lifestyle practices overall, patterns of lower symptom burden, fatigue, depression, and higher QoL were revealed with integrative medicine utilization. Although limited by gender discrepancy and patient reported data, this study may offer a foundation to structure future integrative medicine trials to complement standard therapies in MPN patients.
Gowin:Incyte: Consultancy, Other: Scientific Advisory Board, Speakers Bureau. Mesa:UT Health San Antonio - Mays Cancer Center: Employment; Promedior: Research Funding; NS Pharma: Research Funding; CTI Biopharma: Research Funding; Genentech: Research Funding; Gilead: Research Funding; Incyte Corporation: Research Funding; Novartis: Consultancy; Pfizer: Research Funding; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.