Abstract
Background: Nowadays acute myeloid leukemia (AML) patients above the age of 60 years are often candidates for Allogeneic Hematopoietic Stem Cell Transplantation (HSCT). However, little is known about the outcomes of HSCT in this particular population, due to the low number of HSCT with robust follow-up, the heterogeneity between centers, as well as reports usually mixing AML and other diseases such as myelodysplastic syndrome. We used the database of the Francophone society for stem cell transplantation and cellular therapy to address this question in a large cohort of patients in a recent time period.
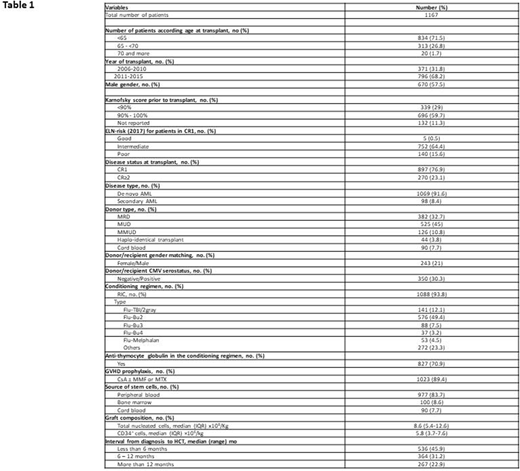
Patients and methods: 1167 consecutive patients aged ≥60 years with AML in complete remission (CR), transplanted between January 1st 2006 and January 1st 2016, reported to ProMISe (Project Manager Internet Server), an internet-based system shared by 36 Francophone transplantation centers, were reviewed. Classical post-HSCT endpoints were studied such as engraftment, acute and chronic graft-versus-host disease (GvHD), non-relapse mortality (NRM), relapse rate, leukemia free survival (LFS) as well as overall survival (OS). Cytogenetic risk was assessed according to the European Leukemia Network 2017 for patients in first complete remission. Data were analyzed using proportional hazards models and proportional sub-distribution hazards models in presence of competing risks.
Results: Patients' Characteristics are detailed in Table 1. The median age at HSCT was 62.9 years (Interquartile range -IQR 61.9-66.1). Patients aged ≥60 years but less of 65 represented 63.8% of the population with 68.2% of patients transplanted in the recent period (2011-2016). Most patient had de novo AML (91.6%), in first CR (76.9%) with intermediate risk (83.8%) according to ELN-2017 classification. A matched unrelated donor (MUD) was used in 45 % of transplants and the majority of patients received peripheral blood stem cells (83.7%). Half of the patients received fludarabine and 2 days busulfan as conditioning regimen. The majority of patients (70.9%) received anti-thymocyte globuline (ATG). Engraftment occurred in 1089 patients (93.3%; 95%CI, 91.9-94.8). Day 100 cumulative incidence of grade II-IV acute GVHD was 24.6% (15.7% grade II; 5.8% grade III; 3% grade IV). At last follow up, 378 patients had developed chronic GVHD (severe in 37.2% of them; 95%CI, 34.0-40.3). With a median follow-up of 3.5 years (95%CI, 3.1-3.7 years), overall survival (OS) and LFS probabilities at 3 years were 50.7% (95%CI, 47.7-54.0) and 44.8% (95%CI, 41.8-48.1), respectively. In multivariable analysis, the only factor associated with worse OS was the use of a mismatched unrelated donor compare to MUD [Hazard Ratio (HR): 1.35 (95% CI, 1.01 to 1.80), p=0.04]. At 3 years, relapse incidence was 34.4% (95% CI, 31.5-37.4). The use of a sibling donor compared to MUD [Sub-distribution Hazard Ratio (SHR): : 1.49 (95% CI, 1.19 to 1.87), p<0.001], poor risk AML in CR1 according to ELN classification [SHR: 1.49 (95% CI, 1.10 to 2.02), p=0.01], as well as the use of ATG in the conditioning regimen [SHR: 1.57 (95% CI, 1.21 to 2.05), p<0.001] were associated with a higher risk of relapse. During the study, 534 patients died (main causes of death was relapse, 53%); leading to a CI of NRM of 20.7% at 3 years (95%CI, 18.2-23.2). A karnofsky score above 90% [SHR: 0.74 (95% CI, 0.56 to 0.98), p=0.04] and the use of a sibling donor compare to MUD [SHR : 0.43(95% CI, 0.30 to 0.63), p<0.001] were associated with reduced NRM.
Conclusion: With more than 3 years follow-up, which is long enough for our results to be considered to be robust, the use of a mismatched unrelated donor was the only factor associated with worse overall survival in this population of AML patients aged of 60 years or more. Relapse appeared as the first cause of death, independently related to AML ELN poor risk classification, but also to the use of a sibling donor and of ATG in the conditioning regimen. This study highlights the major role of alloreactivity in this particular population, where modulation of T-cell alloreactivity as well as donor choice should be urgently addressed in well-designed prospective trials.
Peffault De Latour:Amgen Inc.: Research Funding; Novartis: Consultancy, Honoraria, Research Funding; Pfizer Inc.: Consultancy, Honoraria, Research Funding; Alexion Pharmaceuticals, Inc.: Consultancy, Honoraria, Research Funding. Chalandon:Roche: Membership on an entity's Board of Directors or advisory committees, Other: Travel costs.
Author notes
Asterisk with author names denotes non-ASH members.