Abstract
Introduction:Fibrinolysis plays an important role in the treatment of ST-elevated myocardial infarction (STEMI) when percutaneous coronary intervention is not readily available. Early and successful myocardial reperfusion with thrombolytic therapy effectively reduces the infarct size and improves the clinical outcome. However, the process of restoring blood flow to the ischemic myocardium can induce injury and reduce the beneficial effects of myocardial reperfusion. Previous studies had shown that platelets, leukocytes and TF play important role in thrombotic complications after fibrinolysis in AMI. However, there are still 10-15% patients who have risk for re-occlusion after antiplatelet and anticoagulant therapies. Thus, we speculate that there may be other mechanisms involved in the hypercoagulability after STEMI fibrinolysis. Neutrophil extracellular traps (NETs) are double-edge swords that could ensnare and kill microbial pathogens but also contribute to thrombosis. However, the role of NETs during STEMI fibrinolysis-induced re-occlusion is largely unknown. Our aims were to determine the procoagulant role of NETs after successful thrombolysis, and to elucidate its interaction with endothelial cells (ECs).
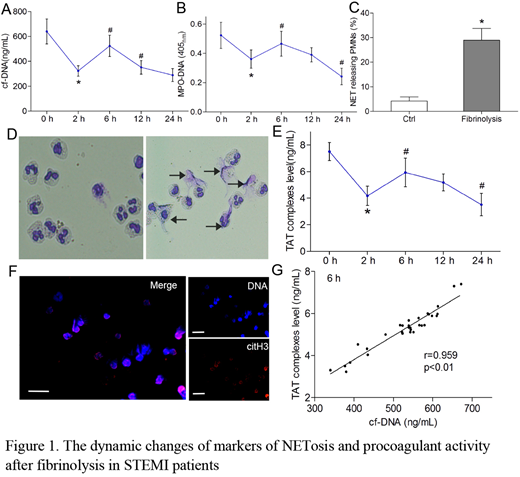
Methods:31 STEMI patients with successfully fibrinolysis and 12 healthy controls were enrolled. Patient blood samples were collected at 0 h, 2 h, 6 h, 12 h and 24 h after fibrinolysis. Cell-free DNA (cf-DNA) was quantified using the Quant-iT PicoGreen dsDNA Assay Kit. ELISA was used to detect MPO-DNA complexes and TAT (thrombin-antithrombin) complexes. Wright-Giemsa and immunofluorescence confocal microscope were used to analyze and quantify NETs formation in neutrophil cells. ECs were incubated in growth media containing 20% pooled serum obtained from healthy donors in the presence or absence of 20-fold concentrated neutrophil extracellular chromatin. The procoagulant activity (PCA) of neutrophils and ECs was measured by clotting time and purified coagulation complex assays. DNase I or anti-TF were included in the inhibition assays.
Results: We found that cf-DNA, MPO-DNA and TAT are significantly reduced at 2 hours in STEMI patients with successful fibrinolysis. Their levels then increased and peaked at 6 hours (Figure 1A, B, E). Interestingly, the level of cf-DNA at 6 hours in STEMI thrombotic patients was positively correlated with TAT (r=0.959; p<0.01; Figure 1G). Wright-Giemsa and immunofluorescence staining showed that NETs were released by STEMI reperfusion neutrophils or by control neutrophils treated with plasma obtained from STEMI patients with fibrinolysis (Figure 1D,F), and the percentage of NETs-releasing PMNs was about 30% (Figure 1C). Isolated neutrophils from fibrinolytic patients in vitro demonstrated significantly shortened coagulation time and increased fibrin formation after 2 hours fibrinolysis, and peaked at 6 hours. DNase I but not anti-tissue factor antibody could inhibit these effects. Co-incubation assays revealed that NETs triggered PS exposure on ECs, converting them to a procoagulant phenotype. Confocal imaging of NETs-treated ECs illustrated that bound FVa and FXa colocalized within PS-enriched areas of ECs to form prothrombinase, and further supported fibrin formation. Moreover, patients with recurrent ischemia showed significantly higher NETs release and thrombin generation than non-recurrent ischemia.
Conclusions: Our study reveals that the PCA of STEMI following fibrinolytic administration decrease after 2 hours, then increase and peak at 6 hours, which is at least partly due to the release of NETs induced by activated PMNs. Additionally, NETs partly contribute to ECs injury after myocardial reperfusion. DNase I can disconnect NETs and may therefore serve as a promising therapeutic target in STEMI reinfarction and recurrent ischemia.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.